Il bando
Per partecipare al concorso, il candidato dovrà, a pena di esclusione, presentare la domanda esclusivamente tramite la procedura telematica all’indirizzo internet https://www.concorsi.unina.it/domandeMaster/ entro e non oltre il termine indicato nella scheda allegata al presente bando e seguire correttamente tutte le prescrizioni indicate nel presente articolo. Decorso tale termine, la procedura telematica sarà automaticamente disattivata e, pertanto, non sarà più possibile iscriversi al concorso.
Collegarsi al sito web di Ateneo: https://www.concorsi.unina.it/domandeMaster/;
Apnea ostruttiva del sonno: una nuova interpretazione per un nuovo trattamento
Gazzetta Medica Italiana – Archivio per le Scienze Mediche 2023 mese;182(0):000–000
DOI : 10.23736/S0393-3660.23.05091-X
OSAS: Obstructive Sleep Apnea : Between myth and reality.
Dott. Antonio Ferrante
Medico Chirurgo, Spec. In Odontostomatologia
Docente Master ”Posturologia clinica” Univ. Pisa, Napoli
Autore di contatto: dott. Antonio Ferrante I trav. Luigi Angrisani, 23 84014 Nocera Inferiore (Sa) Italia e-mail dott.antonioferrante@gmail.com
Key words
OSAS, Trigeminal Nose-Palatine Nerve, Tongue Spot, Surface Electromyography, Neuro-transmitters, Concentration, Memory.
Abstract
The article aims to shed light on an aspect too little considered: the true causes of apnea, purifying it of unverified statements, and referring to clinical, scientific data and linking various information to consider Apnea in a new light, and to outline new courses of treatment. BACKGROUND: Obstructive apnea is a sleep disorder increasing constantly and involves both adult and children. Many causes have been hypothesized, but none of them have been fully validated. The discovery that the nose-palatine nerve (second branch of the trigeminal nerve), presents a huge amount of all five types of postural receptors present in the human body, led us towards a different interpretation. AIM OF WORK: To prove that the Obstructive Sleep Apnea is a consequence of an improper posture of the tongue and of the hypertone from this determined, debunking of the false myths METHODS: We measured the diameter of the faring in profile teleradiographies. RESULTS: we appreciated a steady increase in diameter. CONCLUSIONS: Apnea in many cases is not caused by hypertonicity, but, on the contrary, by linguo-pharyngeal hypotonia, which is treatable by myofunctional re-education.
Background Obstructive apnea is a sleep disorder increasing constantly and involves both adult and children. It brings with it a number of effects on the nervous, metabolic and vascular systems (1). Many specialists have tried to find explanations and treatments, but they are incomplete and unable to explain the complexity of signs and symptoms that this disease presents. A doctor trys to prevent Apnea but desn’t why this disorder appears. So, for example, the biochemical aspect, considering the amount of vitamin D in serum is analyzed (2.3), but without questioning whether such vitamin absorption depends on the specificity of the Ph of the digestive tract. The blood level of Leptin is considered as a sign of the severity of the syndrome, without wondering what neurologically controls leptin. (4) The doctors limited themselves to describe the seriusness of the apnea without making any effort to achieve a etiopathogenesis (5,6,7) An attempt to control the disease was made through rapid palatine expansion, an orthopedic intervention for the maxillary divarication and the recovery of amplitude of the palate (8) or with tonsillectomy (9), but with not always complete results. To reduce or prevent episodes of Apnea the use of C-Pap pressure fans was implemented, which, in our view, can cause damage to the middle and inner ear through the increase of pressure and thus incoraging Tinnitus and Vertigo. In cases do not respond to C-Pap, it has been proposed to intervene surgically to get throat sphincter expansion (10) and even come to advocate the use of maxillary repositioning surgery with of Le Fort operation (11) or with Mandibular Advancement (12).
As a causative factor, the epiglottis collapse (13), pharyngeal muscle hypotones and the accumulation of perifaringeal fat and mandibular retrusion were taken in to account. Meanwhile, some researchers have emphasized the co-morbidity of certain diseases such as obesity, diabetes, hypertension, hypothyroidism (14). We will try to explain later on the relationship that links these elements that are difficult to place in the clinical picture in the absence of particular basic knowledge.
Finally the tongue was taken into consideration and especially the short frenulum, as a cause of apnea. (15) From here starts our observation that will try to explain many misunderstood aspects of the problem to make the syndrome understandable.
It is necessary to give some preliminary remarks for those not familiar with the tongue and its posture. The tongue is the first organ to function in the foetus. It is already completely formed at 51st day of pregnancy, when the rest of the body is simply sketched. Starting from the 13th week of gestation, deglutition is the force for the conformation of the palate; improvement of the swallowing act itself; the functionalization of the digestive tract and kidneys.
In the absence of causes affecting the tongue function as, for example, the presence of an umbilical cord wrapped around the foetus’ neck, multiple pregnancies, incorrect fetal intrauterine positioning, tongue posture tends to be oblique, with the tongue apex in contact with the nose-palatine nerve. This position is determined by the balance of sixteen muscles that make up the tongue, which can be divided into two antagonistic groups: those that carry the tongue up and back (essential for proper swallowing) and those that move it horizontally, both in the postero-anterior direction (almost always hyperactive in an incorrect swallowing) and latero-lateral. In the correct swallow
the tongue rests with the apex on the palate in correspondence with the palatine receptors and gradually lifts the body by pressing it against the palate. This movement is learned and consolidated during the squeezing of the nipple which occurs during breast-feeding. The muscles involved are those with vertical action.
The muscles with a horizontal function are the only ones fully active in the case of lactation with artificial methods (the baby learns to swallow with the teat that compresses the tongue downwards) or in the presence of abnormalities in the shape of the tongue such as the short frenulum and the tongue frankly ankylotic. The lack of contact of the tongue with palatine receptors is, at times so prolonged and total, that a generalized hypertonic can be established able to create a lingual dyspraxis in the newborn and fibromyalgia in an adult.
In order to better understand the essence of the phenomenon of Apneas, we must clarify some aspect of the emerging deal. Everything is born from the discovery that the nose-palatine nerve (the final part of the second branch of the trigeminal nerve, which arises on the palate through the channel of the same name) (Fig. 1), presents a huge amount of all five types of postural receptors present in the human body. The first study is due to professors Halata and Baumann (16) who, at the Institute of Comparative Anatomy of the Hamburg University, found the same receptors in all the animal species studied. On the other hand, at my Myofunctional rehabilitation office, born for orofacial muscle balance and swallowing treatment in orthodontic field, we realized that, whenever we place during rehabilitation the tongue apex in physiological position in contact with the palate, which corresponded exactly to the emergence of the nose-palatine nerve, the subject examined showed apparently unexplained immediate changes in posture and of load distribution breech. The knowledge that by placing the tongue correctly, the Trigeminus was stimulated, allowed us to undertake a research path that is giving enormous results. It is discovered, for example, the importance of stimulation of this place, that has been defined SPOT. A student of the “Master on swallowing function in the postural field” that I coordinated at the Institute of Neurology of the Sapienza University in Rome, called him with an italian acronym Sensor Primitive Oral Trigeminal. This stimulation is fundamental for improving the motor skills and physical freedom in subjects with Parkinson’s disease (17, 18, 19). In two Research Theses we have seen the modification of the electro-encephalographic waves in patients with dysfunctional swallowing, positioning the tongue to the palatal Spot (20) Effects on the presence of epileptic waves have been highlighted. These anomalous waves tend to disappear very frequently when the tongue is placed at the Spot. Just shortly after the Theses produced, an American research was published confirming the goodness of our results, showing how trigeminal dysfunction can underlie many forms of epilepsy. (21)
With surface electromyography it was possible to appreciate the immediate effect on muscle tone with reduction and rebalancing of the muscles of the whole body (Alberto thesis, art. Sucking). The lack of stimulation of the palatine receptors would be the basis of the various forms of muscle hypertonus which, as I said before, can affect the whole organism. Failure to stimulate the palatine receptors is also responsible for the decrease in melatonin secretion. This substance, which in its metabolism is transformed into serotonin, easily dosed through the excretion of 5 hydroxy-indole-acetic acid, check, among others, the rate of production of cortisol which must be secreted during the day, at 8.00 and 15.00. In the absence of melatonin, it is produced at night by coming into conflict with insulin, growth hormone, leptin and ghrelin (the hunger and satiety hormones).
The explanation of all the observations made derives from the study of neurology of the nasopalatine nerve which manages to explain what has been observed. Stimulation of the nasopalatine nerve determines the activation of the brain stem with the production of Serotonin.
The trigeminal trunk, before reaching the mesencephalic Motor nucleus, emits a branch for the Locus Coeruleus which in turn is directly or indirectly responsible for the production of the various neuromediators including, Acetylcholine, Nor-adrenaline, Melatonin and Serotonin from the pineal gland. the lack of which is involved in the alterations of muscle tone, motor skills, sleep, memory. (22).
Theses conducted in the Master in Posturology at the “Sapienza” University of Rome, have shown how the stimulation of the Palatine Spot is able to bring the production of Serotonin back to normal values in subjects suffering from Idiopathic Juvenile Scoliosis (23.24) and a Thesis carried out in the Physiatry and Rehabilitation Clinic of the second University of Naples showed how the positioning of the tongue in the Spot determines an instantaneous reversal of the tested muscles. (25) Ferrante A. and Scoppa F. studies showed instantaneous changes of body posture evaluated with the scoliosometer and the weight bearing platform by stimulating the Palatine SPOT (26.27). This effect is certainly due to a change of cerebellar stimulation through the stimuli that travel the trigeminus, locus coeruleus, cerebellum way. Spot stimulation induces serotonin production, as demonstrated by two theses conducted in the master’s course in posturology, and melatonin production which we know to be correlated with thyroid control and glycemic function.There are over a thousand indexed articles that prove the importance of melatonin in controlling the general function of the organism.
Aim of work:
To prove that the Obstructive Sleep Apnea is a consequence of an improper posture of the tongue and of the hypertone from this determined, debunking of the false myths, that are not based on specific studies, but the fruit of suppositions consolidated by tradition.
In the past it was considered OSAS as determined by hypotonia of oro-faringeal musculature whose collapse would determine the “fall” of the tongue into the pharynx blocking it. (28)
Actually we are carrying out studies that show that the lack of nose-palatine receptors stimulation causes the hypertonus of the musculature of the whole body.
Obstructive apnea is probably a consequence of the jo-glosso muscle hypertonicity that drags the lingual base to the bone joid, associated with the pharynx constrictors hypertonus. The decrease of the pharyngeal lumen justifies the appearance of the obstruction much better than the muscular hypotone. The variation of pharyngeal caliber can be very well appreciated in two successive teleradiography, the first with the tongue in the usual position, the second with the tongue apex in contact with the palatine Spot. If we analyze a patient who has dysfunction of swallowing, the pharyngeal caliber variation can be appreciated very well in the two teleradiographs, the first with the tongue in the usual position, the second with the lingual apex in contact with the palatine Spot. (Fig. 2) The rx clearly shows how much the pharyngeal space is enlarged by positioning the tongue correctly and how the hyoid bone is positioned further down due to the decreased tone of the sub-mandibular muscles. An electro-myographic study conducted by us and in course of publication has shown how the muscular hypertonia often fades to disappear when the tongue is placed in contact with the Spot. (Fig. 3, 4)
These instrumental studies have accompanied the clinical findings that confirm strongly as expressed so far.
Methods
We followed a group of 28 patient suffering from sleep apnoea (between the 47 episodes and 234 per night). The age of the subjects was between 7 and 68 years. All related to our Center for lingual dysfunction problems.
In particular:
11 subjects needed orthodontic treatment ( 9 prepubertal subjects and 2 post pubertal )
3 adults treated for temporomandibular joint problems (TMJ)
6 adults suffered from Tinnitus
8 suffered from muscle-tensive headache or vertebral pain or postural problems (6 adults and 2 children)
Results
Of the 17 adult subjects treated
8 subjects had used CPAP (but only one of them reported improvements with the use of this instrument, as many as 4 people reported the appearance of tinnitus after the start of CPAP use),
4 subjects had use jaw advancers with poor results.
Of the 11 children, only 9 had been monitored by polysomnography, 2 had suffered tonsillo-adenoidectomy.
There was only one subject with very short frenulum, while everyone had received prolonged bottle feeding. Of this group, the little girl with the most serious pathology (continuous headache and apneas 140 per night), after the first 45 days of treatment, had zero episodes of apnea and four episodes of headache, she said of much less painful than in the past.
Within the first two months of re-education only the patient with the short frenulum, who feared to perform the frenulotomy, still presented apneas.
Treated adults have had improvements since the end of the second month of therapy and only two entities that had seen fewer hypertones, but that still had higher values of the standard, reported the presence of sporadic crises.
Conclusions
In light of what has been said, myofunctional re-education, carried out by trained personnel, is able to work on the lingual function and on the damage created by muscular hypertonus which is known as one of the most important and frequent causes of OSAS. From this derives the need to don’t neglect, beyond the evaluation of all the other known causes, also the correct swallowing function as a cause of Apnea.
Given the huge incidence of artificial feeding in the civilized countries and the consequent huge amount of lingual dysfunction (78% of the population), the altered swallowing and its consequences (remember that the low lingual posture and the consequent oral breathing are very often the cause of the problems of adenoids and tonsils, considered themselves causes of Apnee) (Fig. 5,6) a review and eventual treatment of swallowing pathologies is an indispensable complement of every treatment of OSAS.
REFERENCES
1 Perez C.; Obstructive sleep apnea syndrome in children; Gen Dent. 2018 Nov Dec;66(6):46-50. 2 Kirac D, Yagcioglu Yassa O, Gezmis H, Mayda Domac SF, Altunok EC, Genc E; Different VDR, VDBP genotypes and vitamin D levels may effect obstructive sleep apnea syndrome; Cell Mol Biol (Noisy-le-grand). 2019 Jan 31;65(1):46-51.
3 Yassa OY, Domac SF, Kenangil G.; Serum Vitamin D Status does not Correlate with the Severity of Obstructive Sleep Apnea in Male Adults: A Controlled Study Design with Minimized Factors Influencing Serum Vitamin D Levels; Int J Vitam Nutr Res. 2019 Feb 20:1-7
4 Cakir I, Uluhan M; Cardiotrophin-1 and leptin as cardiovascular risk markers in male patients with obstructive sleep apnea syndrome; Arch Med Sci Atheroscler Dis. 2018 Nov 6;3:e123-e128. doi: 10.5114/amsad.2018.79407. eCollection 2018
5 Trachsel D, Datta AN; ;Sleep-Disordered Breathing in Childhood; Praxis (Bern 1994). 2019 Jan;108(2):97-102. doi: 10.1024/1661-8157/a003162.
6 Stöwhas AC, Lichtblau M, Bloch KE.; Obstructive Sleep Apnea Syndrome; Praxis (Bern 1994). 2019 Jan;108(2):111-117. doi: 10.1024/1661-8157/a003198.
7Gelardi M, Intiglietta P, Porro G, Quaranta VN, Resta O, Quaranta N, Ciprandi G; The role of the nasal valve in patients with obstructive sleep apnea syndrome. Acta Biomed. 2019 Jan 11;90(2-S). doi: 10.23750/abm.v 90i2-S.8097.
8 Villa MP1, Malagola C, Pagani J, Montesano M, Rizzoli A, Guilleminault C, Ronchetti R.;
Rapid maxillary expansion in children with obstructive sleep apnea syndrome: 12-month follow-up. Sleep Med. 2007 Mar;8(2):128-34. Epub 2007 Jan 18.
9 Mure C, Blumen M, Alali A, Page L, Chabolle F:Surgical ablation of lingual tonsils in the treatment of obstructive sleep apnea. Eur Ann Otorhinolaryngol Head Neck Dis. 2019 Feb;136(1):19-23. doi: 10.1016/j.anorl.2018.11.001. Epub 2018 Nov 30.
10 Güler İ, Kuzucu İ, Baklacı D, Kum RO, Kum NY, Özcan M; Efficiency of Expansion Sphincter Pharyngoplasty in the Treatment of Obstructive Sleep Apnea Syndrome.
Turk Arch Otorhinolaryngol. 2018 Dec;56(4):206-209. doi: 10.5152/tao.2018.3665. Epub 2018 Dec 21.
11 Ishida T, Manabe A, Yang SS, Watakabe K, Abe Y, Ono T An orthodontic-orthognathic patient with obstructive sleep apnea treated with Le Fort I osteotomy advancement and alar cinch suture combined with a muco-musculo-periosteal V-Y closure to minimize nose deformity. Angle Orthod. 2019 Jan 30. doi: 10.2319/052818-406.1. [Epub ahead of print]
12 Geering S, Broome M, Heinzer R, Lambercy K.; Sleep apnea : diagnostic and therapeutic modalities in case of failure of the CPAP; Rev Med Suisse. 2018 Oct 3;14(621):1751-1754.
13Chen G, Liao WJ, Zhang XW.; Research progress of obstructive sleep apnea syndrome caused by epiglottic collapse; Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019 Feb 5;33(2):186-189. doi: 10.13201/j.issn.1001-1781.2019.02.024.
14 Sweed RA, Hassan S, ElWahab NHA, Aref SR, Mahmoud MI.; Comorbidities associated with obstructive sleep apnea: a retrospective Egyptian study on 244 patients. Sleep Breath. 2019 Jan 26. doi: 10.1007/s11325-019-01783-w. [Epub ahead of print]
15 Guilleminault C, Huseni S, Lo L.; A frequent phenotype for paediatric sleep apnoea: short lingual frenulum; ERJ Open Res. 2016 Jul 29;2(3). pii: 00043-2016. eCollection 2016 Jul.
16 HALATA Z., BAUMANN K.I.: “Sensory nerve endings in the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp 427-437,1999
17 Ferrante A., Scoppa F., Bruzzese F., Guirreri S., Nola D.: Myofunctional therapy in Parkinson’s desease patients. A controlled randomized blind clinical study; ISPGR, p 335, June 2009
18 Ferrante A., Bertoni da Silva, J.G., Bruzzese F., Guirreri S., Nola D., Fin G., Rover C., Daslanora C.T., Nodari R,J.; Efeito da Terapia Miofunctional no tratamento teraputico do mal de Parkinson.Unoesc & Ciencia –ACBS- Ed.Especial, p.47-52, 2014
19 Fetoni V., Guirreri S, Molini G. E., Ferrante A, Sasanelli F.: La Terapia Miofunzionale nella malattia di Parkinson: Studio Pilota; comunicazione XXXIV CONGRESSO NAZIONALE LIMPE, 2007
20 Pagnini P.; Risposte corticali alla stimolazione dello Spot Linguale; Master in Posturologia cl. Univ. Pisa a 2009-2010
21 DeGiorgio C.M., Shewmon A., Murray D., Whitehurst T.; Pilot Study of Trigeminal Nerve Stimulation (TNS) for Epilepsy: A Proof-of-Concept Trial ; Epilepsia,47(7);1213-1215, 2006
22 De Cicco V.; Concetti di Neuro-anatomia e Neuro-fisiologia; cap II pp 11-70, La Nuova Ortodonzia, Marrapese ed. Roma, 2007
23 Locati F., Fedeli R., Correlazione tra Deglutizione scorretta, secrezione di Serotonina e Scoliosi in età evolutiva; Tesi Master in Posturologia Univ Sapienza Roma, 2008-2009
24 Salvatore Tamburro S., Severino A., Nastro S.; Valutazione dei valori urinari di serotonina in ragazzi scoliotici, prima e dopo tre mesi di rieducazione della deglutizione; Tesi Master in Posturologia Univ. Sapienza Roma, 2009-2010
25 Ferrante Al.; Modificazioni posturali secondarie ella variazione della funzione di alcuni muscoli del capo e del collo; Dip. Scienze Ortopediche, Traumatiche, Riabilitative, Plastico-ricostruttive, II univ. Napoli, anno 2006
26 Ferrante A., Reed-Knight E., Bello A., Comentale P.: Variazioni posturali conseguenti a cambiamento della posizione della lingua e a trattamento miofunzionale; Ortognatodonzia italiana , 3, pp 307-315, 2002,
27 Ferrante A., Scoppa F.; Tongue position and postural control. Double blind random study in 360 post puberal subjects; Gait & Posture, vol. 21, suppl. 1, p. 130, June 2005
28 Schlegel J1, Urban PP.; Electrophysiological brain-stem diagnosis in patients with a pronounced obstructive sleep apnea syndrome; Dtsch Med Wochenschr. 1999 May 21;124(20):613-7.
THE SHORT LINGUAL FRENUM AS A RISK FACTOR FOR CEREBRAL VASCULOPATHIES
EJMHR European Journal of Medical and Health Research Volume 1 | Number 3 |November-December 2023
THE SHORT LINGUAL FRENUM AS A RISK FACTOR FOR CEREBRAL VASCULOPATHIES
Dr. Antonio Ferrante, Dott. Roberto M. Crotti
Keywords: Short lingual frenulum, ankyloglossia, Stroke, cerebral ischemia,
Abstract: Introduction: The tongue is the first functioning organ in embryonic development. Its developmental abnormalities can lead to dysfunctions with distant damage. Cranio-cervical anatomy suggests that lingual dysfunction may contribute to damage in the cerebral arteriovenous flow. Objective: To evaluate the possible relationship between a short frenulum and cerebral vascular problems. Method: We conducted an epidemiological study comparing the presence of vascular problems in families where the examined subject had a short frenulum (a genetically transmitted condition) and families in which the examined subject had no frenulum abnormality. Results: The presence of a short lingual frenulum was correlated with the presence of episodes of vascular damage in approximately 80% of cases, while in families without this lingual alteration, the percentage of damage ranged from 10 to 13%. Conclusions: The significant influence that the presence of an altered lingual frenulum seems to have on the future possibility of developing vascular problems should lead to a more careful evaluation of the presence of an incorrect frenulum size.
Introduction: The tongue appears in the embryo at about four weeks in the so-called mesobranchial area. In the same area, the epiglottis, thyroid, submandibular, and sublingual glands also form. However, the tongue mainly originates from the occipital somites, which, along with the formation of the cervical vertebrae, participate in cerebral blood supply through the vertebral arteries. The tongue remains connected to the cervical vertebrae by immersing itself in the cervical fascia, which also contains the hyoid bone and related structures. Another peculiarity of the tongue is that it is the only organ innervated by six cranial nerves.(1) As Professor Marcello Brunelli, the discoverer of the function of cyclic AMP in short-term memory mechanisms (2), pointed out, the tongue is the only organ represented once and a half in each cerebral hemisphere. To understand how a lingual dysfunction may predispose to vascular damage, we must remember the cranio-cervical vascular system and the anatomy and physiology of the tongue and swallowing.
The most important element is probably the Vertebral Artery. This artery has a peculiarity: in its direct path to the skull, it penetrates the vertebral foramina from C6 to the Atlas (C1), after which it deviates backward and enters the Occipital Foramen, where it then anastomoses with the contralateral artery (the Basilar Trunk) near the Roots of the Hypoglossal Nerve. From it originate the Meningeal Branches, the Anterior and Posterior Spinal Arteries, and the Posterior Inferior Cerebellar Artery. The External Carotid Artery, which originates at the level of C3 and C4 and enters between the Posterior Belly of the Digastric Muscle and the Stylohyoid Muscle, is also important. Limiting ourselves to listing only the branches that may be affected by muscle dysfunction related to lingual function, we must mention:
The Ascending Pharyngeal Artery (Pharyngomeningeal), the Occipital Artery, which goes to the muscles of the occipital region superficially and to the meninges, the Medial Meningeal Artery, which ends with a Frontal Branch and a Parietal Branch that distribute internally to the Dura Mater of the respective areas. The Accessory Meningeal Artery.
Internal Carotid Artery. Originating just above the lateral edge of the Thyroid Cartilage, it penetrates the Temporal Bone through the Carotid Foramen, releasing four branches (e.g., Anterior Choroidal Artery, Anterior Cerebral Artery, Middle Cerebral Artery, and Posterior Communicating Artery).
Anterior Cerebral Artery, which gives rise to the Basilar Trunk. It releases Central Branches that penetrate the White and Gray Matter of the underlying nuclei and Cortical Branches that distribute to the Cortex of the Lobes.
Middle Cerebral Artery, which releases Cortical Branches and Central Branches.
Vertebral Vein (Brachiocephalic Venous Trunk). Originating from venous plexuses at the level of the Occipital Bone and C1, it descends within the Vertebral Foramina of the Vertebrae down to C6, after which it heads to its root. It provides blood drainage for the Spinal Cord and the Cervical Vertebral Column.
External Jugular Vein (Subclavian Vein). Its two roots, the Retromandibular Vein and the Posterior Auricular Vein, meet and converge approximately behind the Mandibular Angle.
Venous Sinuses of the Dura Mater. These are dilated venous structures located in the Dura Mater of the Skull, which receive various venous vessels. They then mostly drain into the Internal Jugular Veins.
Superior Cerebral Veins, draining the upper medial part of the Cerebral Hemispheres. They join to form the Superior Sagittal Sinus, which is located at the point where the Saggital Suture ends.
Analogous Inferior Cerebral Veins, which collect blood from the Occipital Lobes and Temporal Lobes. From the base of the Brain, it heads toward the Tentorium.
Sphenopalatine Vein, which drains the Nasal Cavity and communicates with the Ophthalmic Vein.
Internal Jugular Vein, which carries blood from the Brain and communicates with the Subclavian Vein. Its lower part is also called the Venous Angle.
Subclavian Vein, which becomes the Brachiocephalic Trunk in conjunction with the Internal Jugular Vein.
The preceding description demonstrates that not only arteries but also veins and venous sinuses may be affected by cranial dysfunction due to lingual dysfunction. The appearance of vascular phenomena in areas far from the tongue should therefore not be surprising. These considerations prompted the evaluation of the influence that a lingual dysfunction, such as a short frenulum, can exert on the cranio-cervical region.
THE LINGUAL FRENUM Along the midline, there is a thin fold of fibro-mucous membrane, the lingual frenulum, which connects the body of the tongue to the mucosa of the oral floor. The lingual insertion can be at the tip, and this pathological condition is called ankyloglossia, or it can be slightly closer (less than 2 cm) or further away (more than 2 cm) from the tip. The alveolar insertion can be marginal, at the base of the tooth, apical, at the apex of the tooth’s root, or subapical, below the apex of the tooth. The presence of a short lingual frenulum can be responsible for limited tongue mobility.
3.1. FUNCTIONAL ANATOMY The tongue, as a functional matrix, plays a plastic role on the palatal vault and the development of the maxillaries. A lingual dysfunction caused by an anatomical impediment such as a short frenulum can create disharmony in the stomatognathic system by altering the relationships between the bony bases and both anterior and posterior stability, causing abnormal tensions on the hyoid bone and, secondarily, cervical and postural issues.
In the resting position, the tip of the tongue comes into contact with the estereceptors, which were discovered only in 1999 to be present in large quantities at the opening in the palate of the nasopalatine nerve, the terminal branch of the second branch of the trigeminal nerve. Discovered by Professors Halata and Bauman, researchers in Comparative Anatomy (3), we have explained in numerous studies that demonstrated their particular importance in the production of neurotransmitters involved in brain function (4,5). In physiological swallowing, the tongue makes contact with the palate at this point (Palatal Spot) with its tip and raises the dorsum, pushing the bolus toward the pharynx (6). Recent research on the function of nasopalatine receptors has shown that their stimulation is also essential for muscle relaxation (7). The lack of contact between the tongue and the palatal receptors, on the contrary, leads to worsening muscle hypertonicity.
A short lingual frenulum, even in a static situation, causes a problem in the lingual and suprahyoid muscles similar to what a short muscle fascia does to the muscle it contains, i.e., contraction or hypertonia. In a dynamic situation, such as during swallowing, it has different effects on the muscles involved, in particular:
- It acts as an anterior anatomical restraint for the stylohyoid and digastric muscles, preventing them from moving the hyoid bone upward and backward, as should occur in physiological swallowing, thus pulling on the styloid and mastoid processes of the temporal muscle and blocking the hyoid bone anteriorly.
- It prevents the styloglossus and palatoglossus muscles from bringing the dorsum of the tongue into contact with the palatal vault.
- It does not allow the subhyoid muscles to perform their important stabilizing function on the hyoid bone, resulting in flexion of the cervical spine and head.
CEREBRAL VASCULOPATHIES In industrialized countries, cerebral vasculopathies are the third leading cause of death, after cardiovascular diseases and neoplasms, but they are the leading cause of chronic disability. The nosological category of cerebral vasculopathies includes both acute conditions, such as cerebral stroke and subarachnoid hemorrhage, and a variety of subacute or chronic clinical conditions, such as subcortical white matter pathologies, vascular etiology cognitive and behavioral disorders, vascular epilepsy, genetically-based vasculopathies, arteriovenous malformations, alterations of the arterial wall of the carotid and vertebrobasilar circulations, and post-stroke recovery and rehabilitation phases. In Italy alone, there are approximately 200,000 acute stroke events each year, with at least 80% being first events, resulting in a one-year mortality rate of 30% for ischemic forms and 50% for hemorrhagic forms. Acute cerebral vasculopathies cause more deaths (1.45 times) than myocardial infarction. In the case of arterial obstruction, ischemic stroke occurs (accounting for approximately 80% of stroke cases). In the case of a rupture of a cerebral artery, cerebral hemorrhage (10-15% of cases) or subarachnoid hemorrhage occurs, and these two situations cannot be differentiated based solely on clinical criteria; they require the use of imaging techniques such as brain CT and MRI. When neurological deficits completely resolve within 24 hours (generally within 60-90 minutes), it is referred to as a transient ischemic attack (TIA) if neuroimaging is negative, or as a completed infarct with full recovery when imaging reveals a vascular lesion consistent with clinical findings.
Despite constituting only about 2% of total body mass, the brain receives 15% of the cardiac output and continuously consumes 20% of the glucose and oxygen available to the entire body. The supply of these nutrients is essential because the brain parenchyma has no energy reserves. Cerebral circulation, through autoregulation systems involving changes in arteriolar resistance, is capable of maintaining relatively constant blood flow that satisfies neuronal energy and metabolic demands, even under conditions of systemic blood pressure variability. When an arterial vessel becomes occluded, blood flow is almost completely interrupted in the central (core) area of the irrigated territory, resulting in neuronal death. In the adjacent area (ischemic penumbra), blood supply is partially supported by collateral circulation, allowing nerve cells to remain vital but damaged and functionally compromised. Neuronal damage is caused by the cessation of metabolic processes, as well as by complex pathophysiological processes such as the release of excitatory neurotransmitters with excitotoxicity, electrophysiological alterations, production of free radicals, which can transform reversible ischemic penumbra into irreversible infarction.
An explanation of the relationship between lingual dysfunction and vascular problems comes from an understanding of the muscular structures.
MUSCULAR RELATIONS (8,9) The thoracic inlet is the region that connects the cervical and thoracic areas; it is crossed by blood and lymphatic vessels in their passage. If the return of cranial fluids to the thoracic cavity is even slightly inhibited by abnormal muscular hypertonicity at the level of the thoracic inlet, cranial movement activity is consequently altered by fluid congestion inside the cranial vault. At the thoracic inlet, the fibers of the sternocleidomastoid and trapezius muscles, along with their fasciae, have a significant impact on the functional mobility of bony structures, as well as on fluid circulation and fascial mobility. Even the infrahyoid muscles and their fasciae can interfere with the normal mobility of these regions, as well as the scalene muscles, which, although not acting directly on the cranial bones, can interfere with blood circulation through the subclavian artery and vein that pass between the fascial layers.
The external and anterior jugular veins are completely enveloped by the superficial layers of these fascial coverings, so an increase in fascial tension due to muscular hypertonicity can result in increased venous backpressure in the cranial vault.
CONSIDERATIONS From the biomechanical analysis of the swallowing process with a short frenulum, it is evident that there is a correlation between this and the state of hypertonia and hypertrophy of part of the infrahyoid musculature and the cervical tract. This evidence suggests that venous flow, although regulated by fine autonomous mechanisms, may encounter difficulties with a dual effect:
- At the arterial level, greater winding of the flow leads to increased sedimentation in areas of difficult passage, resulting in atherosclerotic deposits and increased intravascular pressure.
- At the venous level, the difficulty of passage leads to stagnation of reflux blood, increasing pressure in upstream structures.
DURAL RELATIONSHIPS The dural membrane adheres to the entire inner aspect of the cranial cavity, allowing the passage of various venous sinuses: the sagittal and transverse sinuses, the occipital sinus, the petrosal sinuses, and the straight sinus. The dural membrane transmits tensions originating from any of its points through its own structure, along a direction determined by the geometry of its anchoring points. It is not difficult to imagine how abnormal tensions in the membrane can interfere with the normal movement of cranial bones and the free circulation of blood through the venous sinus system. Interferences with venous sinus drainage can lead to increased intracranial venous backpressure, which reduces normal blood supply to the brain and can also cause a modest but significant increase in cerebrospinal fluid pressure, interfering with the normal movement of these vital fluids through the brain’s ventricular system and various subdural spaces.
TRIGEMINO-CARDIAC REFLEX Observations in humans have shown that overstimulation of the trigeminal nerve (10) can also cause severe bradycardia, hypotension, apnea, and gastric hypermotility. These effects have been attributed to the so-called “trigemino-cardiac reflex” (11,12,13).
The trigemino-cardiac reflex (TCR) is described as the sudden onset of cardiovascular effects (bradycardia, hypotension) that can be accompanied by apnea and gastric hypermotility during manipulation of one of the branches of the trigeminal nerve. It has been described in humans during craniofacial and maxillofacial surgery (Cha et al., 1999) and resection of pontocerebellar tumors (Schaller et al., 1999). Despite the powerful effects of the trigemino-cardiac reflex, there is limited information on the underlying physiological mechanisms.
CONSIDERATIONS The trigemino-cardiac reflex associates trigeminal stimulation with a drop in blood pressure in the cerebral vascular circulation. In the case of a real short frenulum, where the tongue does not reach to stimulate the emergence of the sphenopalatine branch of the trigeminal nerve, part of the trigeminal input is missing. This deficiency can be compensated by overstimulation of the periodontal trigeminal innervation, but it may not be sufficient, resulting in increased intravascular pressure in the cerebral circulation.
RESEARCH Two parallel studies were conducted in two regions of Italy. Patients were evaluated by specialists in orofacial rehabilitation and deglutition. An epidemiological study was conducted. All patients who came to our studies were asked if there were any cases of cerebral vascular diseases in their families, including parents, siblings, aunts, and grandparents. Responses to our question were very different between the group of patients who did not have frenulum problems and those who had a very short frenulum or ankyloglossia (the most severe condition in terms of tension and the ability to express correct motility).
In both studies, the control group consisted of patients undergoing therapy for incorrect swallowing but without lingual structural abnormalities.
The study group in Campania consisted of 40 subjects with a very short frenulum or ankyloglossia. For the control group, 40 subjects were randomly selected.
The study in Tuscany was conducted on 30 people with a real short frenulum according to the protocol described above. A control group of 30 subjects without lingual abnormalities was randomly selected.
Patient Ages: Given the relevance of family history, age was not considered as a significant factor.
RESULTS Of the 40 subjects with a short frenulum in the study conducted in Campania, 31 reported a family history of vascular events, while in the group without a short frenulum, only 4 subjects had a family history of such conditions.
In the study conducted in Tuscany, it was found that out of 30 patients with a real short frenulum, 24 had a family history of various types of vasculopathies, such as stroke, transient ischemic attack, and cerebral hemorrhage, accounting for 80% of the total. Among patients with a normal-sized lingual frenulum, the presence of familial vasculopathies was found in 4 out of 30 subjects (13.3%).
Given the significant value observed, we visited patients admitted to rehabilitation centers after suffering significant cerebral vascular problems. Seventy percent of them had a very short frenulum or ankyloglossia. Considering that approximately 8% of patients die during the first event, this confirms the magnitude of the damage that an altered frenulum can cause.
CONCLUSIONS The research has shown that there are anatomical conditions in which the hemodynamics of cerebral blood flow can be disturbed by an unsupported swallowing pattern with a lack of trigeminal stimulation through the palatal spot. In clinical practice, there is a higher incidence of cerebral vasculopathies when a real short frenulum is present. Furthermore, it leaves open the possibility of further investigations to determine whether appropriate frenulum treatment and swallowing rehabilitation can lead to changes in blood circulation.
BIBLIOGRAFIA
- FERRANTE A. La nuova Terapia Miofunzionale; ed. Centro terapia Miofunzionale, pp. 25-27
- KANDEL E. C. Alla ricerca della memoria. Codice Ed pag. 231
- HALATA Z., BAUMANN K.I.: “Sensory nerve endings in the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp 427-437,1999
- FERRANTE A, FERRANTE Al., FERRANTE C. A new contribution to the knowledge of Adolescent Idiopathic Scoliosis (AIS); vol . 8, issue 3, june 2023; PP 181-192
- FERRANTE A. A new hypothesis to explain the mechanism that may be involved in the genesis of sleep bruxism (SB); Gazzetta Medica Italiana – Archivio per le Scienze Mediche; 2021 September; 180(9):399-403
- FERRANTE A., Manuale pratico di terapia miofunzionale, Marrapese editore, Roma, 2004; 19-32
- FERRANTE A, FERRANTE Al., FERRANTE C. Reflection on Fibromyalgia – A New Interpretation; International Journal of Research in Medical and Clinical Science ; Vol.1, Issue 2, 2023 PP:08-13
- LOCKHART, HAMILTON, FYFE, Anatomia del corpo umano, Casa Editrice Ambrosiana, Milano, 1978: 165-170
- MARTINI, TIMMONS, TALLITSCH, Anatomia umana, EdiSES, Napoli, 2000: 274, 669-672
- CONTI M., “Effetti dell’attivazione propriocettiva del nervo trigemino sul microcircolo piale nel ratto”; Tesi laurea in Neurobiologia, univ. Pisa, 2010;
- SCHALLER B, FILIS A, SANDU N, BUCHFELDER M; Peripheral trigemino-cardiac reflex.Trigemino-Cardiac-Reflex Examination Group (T.C.R.E.G.).Acta Neurochir (Wien). 2009 Dec;151(12):1727. doi: 10.1007/s00701-009-0390-6. Epub 2009 May 26.
- SANDU N, CHOWDHURY T, MEUWLY C, SCHALLER B. Trigeminocardiac reflex in cerebrovascular surgery: a review and an attempt of a predictive analysis. Expert Rev Cardiovasc Ther. 2017 Mar;15(3):203-209. doi: 10.1080/14779072.2017.1286983. Epub 2017 Feb 4.
- CHOWDHURY T, MEUWLY C, SANDU N,CAPPELLANI RB , SCHALLER B Coronary spasm in neurosurgical patients and role of trigeminocardiac reflex. Neurol Res Int. 2014:974930. doi: 10.1155/2014/974930. Epub 2014 Jan 27.
The Importance of the Naso-Palatine Nerve for the Body’s Homeostasis
Volume 1 Issue 1 – 2023
Antonio Ferrante
Spec. in Odontostomatologia, Docente Master in Posturologia Università di Pisa, Università “Federico II “ Napoli
Correspondence: Antonio Ferrante, Spec. in Odontostomatologia, Docente Master in Posturologia Università di Pisa, Università “Federico II “ Napoli, Prima trav. Luigi Angrisani, 23 – 84014 Nocera Inferiore, Email dott.antonioferrante@gmail.com
Received: November 09, 2023 Published: November 25, 2023
Citation: Antonio F. The Importance of the Naso-Palatine Nerve for the Body’s Homeostas. HOJ Emerg and Int Med. 2023;1(1):56–58.
Copyright: ©2023 Ferrante. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and build upon your work non-commercially.
When thirty years ago I approached the re-education of swallowing, perhaps only the name of the nasopalatine nerve was known and that it was the oral terminal branch of the second branch of the trigeminal nerve. It was so little considered that many implantologists, having to insert implants in the premaxilla, eliminated it with impunity without knowing if this would cause harm to the patient.
The interest in this nerve arose when, starting from the second-third month of swallowing re-education, apparently inexplicable improvements began to be appreciated, even before the results on lingual movement and muscle tone. Patients often asked me whether it was due to re-education that vision improved unexpectedly or that a scoliotic spine was so improved that it no longer required the expected treatment with a brace. I had no answers, but the frequency of the improvements found led me to focus my attention on the point that proved to be the means of improvement. It was the nasal-palatine foramen, the emergence of the nerve in the palate and already considered to be the “lingual spot”, the point where the lingual apex must rest to initiate physiological swallowing. I bought anatomy books, magazines in the hope of having an “explanation”, but without finding answers. In 2000 I happened to read in an Anatomy and Embryology magazine, the article written by two professors of Comparative Anatomy, who had found in all higher animals, the presence, at the emergence of the nasopalatine nerve, of an enormous quantity of the 5 major exteroreceptors present in the human body.1 It was the answer I was looking for, the neurological explanation of the improvements seen and not explained. In the meantime, a book of mine, written to warn dentists against carrying out treatments without considering oral muscle function due to the risk of creating problems outside the dental field, had become a textbook in the Masters in Posturology of various Italian universities and I was invited to participate as a teacher. This allowed me to begin a journey of research that perplexed or shocked those who read it. The function of the nasopalatine nerve has come to the fore forcefully both in the postural field and in general medicine. Help in accessing the neurological field came from the presentation at a conference of the case of a volleyball player who, after receiving a ball in the face, found herself with an apparently paralyzed leg, after a hospital stay, in which she had been hypothesized tibial hyperostosis, a neuropathy, a tumor in the spinal cord, a psychosis, he had finally seen the possibility of walking without crutches by sucking the finger (we have shown that you suck to activate the receptors) ( ) or by positioning the tongue on the palatine receptors.
This case captured the attention of Prof. Marcello Brunelli, who,when he worked at the Columbia University laboratory directed by Eric Kandel, had discovered the basis of long-term memory; later director of the Institute of Physiology of the CNR and of the Department of Physiology and Biochemistry of the University of Pisa. He was so interested in the case that he soon became our contact on the relationship between the mouth and the brain. The study of neurotransmitters has given rise to research that ranges across the various fields of medicine.
Among the first, one, taken up by the Santa Caterina University in Brazil ,2 investigated the improvements in parkinsonian patients obtained with stimulation of the nasopalatine spot carried out three times a day for three minutes for three months. The results stunned specialists and a poster, presented at the 2007 National Parkinson’s Congress indicated Myofunctional Therapy as a new means of treating Parkinson’s.
Studies have addressed the effects on serotonin secretion. The interest arose from the improvement of patients with juvenile idiopathic scoliosis by re-educating swallowing for orthodontic problems. Since the effects of serotonin and melatonin deficiency in scoliotic children have been known since the 1990s,3 we assumed that the improvements obtained with re-education were due to an increase in their secretion. We have conducted research ( ) which clarified how palatal stimulation is even capable of tripling serotonin production in just a few months.
Since serotonin is implicated in the control of muscle tone (a research has just been submitted for publication), we hypothesized an interpretation that goes against any previous interpretation for sleep apnea (OSAS). These were explained by a muscular hypotonus with fall of the soft palate towards the pharynx. We have demonstrated, by measuring the diameter of the pharynx in profile radiographs taken with the tongue in the usual position, away from the palate, and with the tongue in contact with the palatine receptors, that it is instead a case of hypertonicity of the pharyngeal constrictor muscles which restrict the pharynx and together with the hypertonicity of the M. Hyoglossus make the passage of air difficult.4
A particular finding was seen in women with difficulty starting a pregnancy, visited for problems with TMJ or for orthodontic requests. I leave aside the relationships between impaired swallowing and orthodontic problems because they can be found in my other articles or books, but I focus on this effect of muscular dysfunction because infertility could hardly be associated with incorrect swallowing. When we realized that the oral problem caused a decrease in Melatonin5 and that, in its absence, prolactin increases, which inhibits the bursting of the follicles, we spoke to the gynecologists, but they ignored us. We then wrote to Prof Eric Kandel, Nobel Prize winner for Neuroscience in 2000. He immediately replied: “Rejoice! In a world of the blind, he who has only one eye is a king!”
The normalization of the electroencephalographic waves was appreciated by correctly positioning the tongue. Enormous changes in functional resonances were also appreciated by placing the tongue on the spot with an increase in active areas. The resonances explained to us the improvements obtained in particular and inexplicable problems. An example: 42 month old child, doesn’t speak, doesn’t walk, drools. Diagnosis carried out in highly specialized centers: atrophy of the corpus callosum. The mother wants me to see it, but I tell her that it’s not my responsibility. She insists and finally takes him for a visit. I explain to her that I am not a neurologist and that the specialists didn’t know what to do, but I feel sorry for her so I tell her that, if the child can move his tongue voluntarily, he will be able to undergo re-education at the age of 6 and stop drooling. An idea comes to me. Does the child like Nutella? (a spreadable hazelnut cream). I ask the mother to apply it to the spot several times a day, especially if when she applies it she finds the palate very clean, a sign that the baby can lick the cream. After a week I get the first email. The child walks holding hands and says simple words. He continues the application and after a month he climbs into bed and asks his mother questions to the disbelief of those who treat him at the Institute.
We are currently studying the effects on the thyroid and the improvements in athletes. There is so much to discover and explain, but there is no doubt that before the appearance of drugs the body was able to rebalance itself naturally.
References
1. Halata Z, Baumann KI. “Sensory nerve endings in the hard palate and papilla incisiva of the rhesus monkey”. Anatomy and Embriology. 1999;199(5):427-437.
2. Bruzzese F, Guirreri D, Nola D, et al. Bertoni da Silva J.G. Efeito da Terapia Miofuncional no mal de Parkinson et al; Unoesc & Ciência ACBS de Editora Unoesc.
3. Machida M, Murai H, Miyashita Y, et al. Pathogenesis of idiopathicscoliosis. Spine. 1999;24:1985–1989.
4. Ferrante A. Apnea ostruttiva del sonno: una nuovainterpretazione per un nuovo trattamento. Gazzetta Medica Italiana – Archivio per le Scienze Mediche. 2023;182(0):000–000.
5. Ferrante A, Ferrante C. L’importanza della corretta informazione trigeminale in casi di difficoltà ad iniziare una gravidanza ; Giorn. It. Ost. Gin. Vol. XXXVIII – n. 3Maggio-Giugno. 2016.
The Physiological Control of Muscle Tone: The Effects of Naso-Palatine Stimulation
Ferrante A.1, Ferrante Al.2, Ferrante C.3
1Centro Terapia Miofunzionale, Italy.
2,3Casa di cura Hermitage Capodimonte, Italy.
Abstract
Purpose of the Study: To evaluate the importance of stimulating the naso-palatine receptors as controllers of physiological muscle tone and the potential effect of their stimulation on improving postural problems.
Methods: Blood tests were used to measure serotonin metabolites in urine, tools for assessing muscle tone (electromyograph), scoliosometer, and baro-podometric platform for postural evaluation. Fluorescein was used, according to the Payne technique, to assess swallowing.
Results: Stimulation of the naso-palatine trigeminal receptors showed improvement in the conducted tests, rebalancing of muscle tone, and a decrease in hypertonia, unlike tongue positioning in contact with other areas of the mouth, which did not show clear and appreciable changes.
Conclusion: Stimulation of the naso-palatine receptors has been shown to be the physiological mechanism for controlling general muscle tone. Lack of stimulation leads to an increase in muscle tone.
Keywords: Muscle Tone, Swallowing, Trigeminal, Naso-Palatine Receptors, Scoliosis.
Purpose Of The Study
In my research across various internet libraries seeking information on muscle tone control, I realized that there are publications on tone measurement (1), others evaluating the effects of various substances on tone variations (2, 3, 4), many studies on substances naturally secreted by the brain, as well as pharmacological substitutes regulating central tone (5, 6, 7). Studies on the relationship with posture and gait movement were found (8, 9). The only studies that we found interesting because they align with our view of the problem are those focused on the study of the effects of serotonin and norepinephrine at the hypoglossal nucleus (10, 11). We found nothing, and I believe that little or nothing has been written about the neurological control mechanism of general muscle tone in healthy individuals in everyday life. This led to the idea of sharing what we consistently observe daily in our work, which could aid in explaining the pathogenesis of some common bodily ailments and the targeted choice of their causal treatment. It all began with a study conducted to explain the postural improvements obtained “involuntarily” during the rehabilitation of lingual function in patients with impaired swallowing mechanisms.
A brief explanation is needed for those who are not fully aware of the swallowing mechanisms. The tongue is the first active organ in the human body (it is functional from the 51st day of pregnancy), and it is the only one related to six cranial nerves. It has a representation in the cerebral cortex far superior to any other organ, composed of eight pairs of muscles with specific functions in both speech and swallowing.
*Corresponding Author: Antonio Ferrante, Centro Terapia Miofunzionale, Italy.
International Journal of Research in Medical and Clinical Science
Volume 1, Issue 2, 2023, PP: 53-57
www.journalserapublications.com
Research Article
The Physiological Control of Muscle Tone: The Effects of Naso-Palatine Stimulation
Ferrante A.1, Ferrante Al.2, Ferrante C.3
1Centro Terapia Miofunzionale, Italy.
2,3Casa di cura Hermitage Capodimonte, Italy.
Abstract
Purpose of the Study: To evaluate the importance of stimulating the naso-palatine receptors as controllers of physiological muscle tone and the potential effect of their stimulation on improving postural problems.
Methods: Blood tests were used to measure serotonin metabolites in urine, tools for assessing muscle tone (electromyograph), scoliosometer, and baro-podometric platform for postural evaluation. Fluorescein was used, according to the Payne technique, to assess swallowing.
Results: Stimulation of the naso-palatine trigeminal receptors showed improvement in the conducted tests, rebalancing of muscle tone, and a decrease in hypertonia, unlike tongue positioning in contact with other areas of the mouth, which did not show clear and appreciable changes.
Conclusion: Stimulation of the naso-palatine receptors has been shown to be the physiological mechanism for controlling general muscle tone. Lack of stimulation leads to an increase in muscle tone.
Keywords: Muscle Tone, Swallowing, Trigeminal, Naso-Palatine Receptors, Scoliosis.
International Journal of Research in Medical and Clinical Sciences
54
Journals Era Publications
It is necessary for the body’s development that its function is perfect. Unfortunately, many factors can affect its mobility: anatomical factors (short frenulum, ankylosed tongue), functional factors (issues related to birth and, especially, artificial feeding methods). In normal swallowing, a newborn learns to swallow after an initial fetal phase in which it begins to move, sucking milk from the mother’s nipple. During this movement, the nipple is compressed and squeezed against the palate to stimulate milk ejection. The point of contact of the nipple with the palate is right at the emergence of the naso-palatine nerve. Agglomerates of all exteroceptors related to postural control function were found at this point, present diffusely on the soles of the feet and, instead, gathered in an area of about ½ cm2 (12). Artificial feeding and the use of pacifiers (necessary to stimulate palatine receptors once the tongue becomes ineffective) increasingly keep the tongue away from the palate and, by reducing the activity of elevator muscles, make it unable to stimulate palatine receptors. In re-educating swallowing, the lingual musculature is tonified in a balanced way (requiring 3 to 4 months), restoring tone to the elevator muscles. In a second phase, the correct swallowing movement is taught, and in the final phase, the new swallowing engram is consolidated. It was incredible for us that many patients who came to our attention for orthodontic reasons, where orofacial muscle imbalance was considered the primary cause of orthodontic damage, unexpectedly improved their postural attitudes and scoliotic curves, if present, within a few months, by practicing only lingual re-education exercises. The idea that the change could be attributed to changes in the tone of paravertebral muscles was clear to me, as I teach in posturology master’s programs, but I come from a dental background. My lack of specific knowledge led me to involve a physiatrist specialist and delve into the issue with a completely fresh perspective, without biases from past knowledge, often unconfirmed by science. The use of laboratory tests as a means to quantify the damage came from a study I conducted to verify the reliability of surface electromyography in measuring muscle tone. I found papers by Machida and others (13, 14, 15, 16), which explained idiopathic scoliosis with a deficiency of serotonin and melatonin. Receptors for these neurotransmitters were found along the entire spinal column, and 5-hydroxyindoleacetic acid, a serotonin metabolite, was found to be low, explaining the tone alterations and muscle imbalance. This observation indirectly suggested that the improvements observed in our patients could probably be attributed to improved serotonin and melatonin production. We then conducted theses (17, 18) at the Posturology master’s program at Sapienza University of Rome to understand if the re-education of swallowing function with the restoration of tongue contact with naso-palatine receptors could increase serotonin production. The results were very encouraging. Three months of placing the tongue apex in contact with palatine receptors for 3 minutes three times a day were able to normalize urinary 5-hydroxyindoleacetic acid values in approximately 70% of the subjects tested, along with postural improvements (19). We also conducted research on a new interpretation of fibromyalgia, considered the result of persistent hypertonicity leading to muscle fiber alterations but accompanied by symptoms unexplainable with previous knowledge (20). At this point, we wanted to understand if all improvements could be attributed to the effects of neurotransmitter production and whether there was an instant effect on the cerebellum, whose paramedian parts receive indirect trigeminal innervation of a reflex nature, due to the central response to naso-palatine receptor stimulation. For this purpose, we conducted tests on the scoliosometer with the tongue in its usual position and then in contact with the receptors (in myofunctional therapy, this point is defined as the “Spot”) (scoliosometer figure). We then tested a group of 10 healthy subjects with incorrect swallowing, no short frenulum, no orthodontic problems treated in any way, aged between 14 and 35 years. Another group of similar subjects in terms of age and dysfunction served as a control group.
Methods
The tools used in the research were as follows:
• For Serotonin Measurement : Control of 24-hour urine 5-hydroxyindoleacetic acid excretion
• For Evaluating Lingual Movement During Swallowing : 1% fluorescein was used, placed at the tongue apex and at two lateral points in the middle part of the tongue (19). The points of contact between the tongue and various oral areas were highlighted using a Wood lamp that causes fluorescein to fluoresce, making the points where the tongue made contact with the oral areas visible.
• For Postural Evaluation: Scoliosometer, also known as a postural analyzer, was used to highlight changes
International Journal of Research in Medical and Clinical Sciences
55
Journals Era Publications
produced by the correct positioning of the tongue on both the frontal and sagittal axes, along with a baro-stabilometric platform called Diagnostic Support.
• For Muscle Evaluation: Surface electromyograph K7 Myotronics
Results
Serotonin Level Examination The examination showed increases in 5-hydroxyindoleacetic acid levels in urine in both males and females, with small variations related to gender. This increase was particularly evident in patients who initially had low values. Improvement was observed in approximately 70% of the subjects, with the most significant result occurring in a female who saw her value increase from 56 micrograms/24 hours to 153 micrograms/24 hours.
Baropodometry
The results obtained from measuring plantar support using a baro-podometric platform are undoubtedly very interesting and conclusive. A sample of ten patients aged between 14 and 35 years was assessed in a static position, first with the tongue in its usual position and then with the tongue positioned at the palatine spot. Another sample of ten patients within the same age range was evaluated simultaneously in a static position with the tongue in its usual position. However, being a control group, they repeated the examination with the tongue not against the Spot but against the lower incisors. In this group, only one person had correct swallowing, and we indeed found deterioration in all parameters.
The parameters considered were
• The ratio of support on the hindfoot to support on the forefoot
• The ratio of support on the right foot to support on the left foot
Results for the Work group (tongue at the spot)
1. Hindfoot/forefoot ratio
Improvement in 10 out of 10 subjects
2. Load distribution ratio between the right foot and left foot
Improvement in 8 out of 10 subjects No improvement in 2 out of 10 subjects
Results for the Control Group (tongue against lower incisors)
1. Hindfoot/forefoot ratio
Improvement in 3 out of 10 subjects. No improvement in 2 out of 10 subjects. Deterioration in 5 out of 10 subjects.
2. Right foot/left foot support ratio
Improvement in 3 out of 10 subjects. No improvement in 2 out of 10 subjects. Deterioration in 4 out of 10 subjects
Electromyography
Through the use of surface electromyography, the resting activity of certain head and trunk muscles and the changes undergone as a result of repositioning the tongue at the palatine spot were evaluated. Subsequently, the same examination was performed on a control group, assessing muscle activity at rest and positioning the tongue against the lower incisors. Four pairs of muscles were assessed: the masseters, sternocleidomastoids, trapezii, and paraspinal muscles at the level of the third lumbar vertebra. Recordings were made with patients in a seated position, without them being informed about the expected outcome of the examination.
Figure 1. Electromyography with the Tongue in the usual position (away from the palate)
Figure 2. Electromyography with Tongue in contact with palatal receptors
56 International Journal of Research in Medical and Clinical Sciences
Journals Era Publications
Reference values and standard deviations for each muscle, defining the degree of activity, will be reported later:
Muscle Reference
Standard Deviation Masseter 1.87 microVolts 1.46
Sternocleidomastoideo 1.98 microVolts 1.75
Trapezi 2.78 microVolts 3.03
Paraspinal L3 1.41 microVolts 1.62
All ten subjects in the active study group presented an improvement and rebalancing of muscle tone, as evidenced by a reduction in values measured during the test with the tongue in its usual position, when it was placed at the palatine spot (Fig 1, 2). The ontrol group subjects showed variable values, with no clear improvement.
Conclusion
The results of the research, consistent with what we have observed daily in our patients over the past thirty years, lead us to affirm that tongue stimulation of the naso-palatine receptors in a resting state and, even more so, during the act of swallowing, represents a natural and physiological means of rebalancing the body’s muscle tone.
Bibliography
Gurfinkel, V.S., Cacciatore, T.W., Cordo, P.J, Horak F.B., 1. (2014) Method to measure tone of axial and proximal muscle. J Vis Exp. 2011 Dec 14;(58). pii: 3677. doi: 10.3791/3677.
Xu, K.S., Yan, T.B., Mai, J.N., (2006) Effects of botulinum 2. toxin guided by electric stimulation on spasticity in ankle plantar flexor of children with cerebral palsy: a randomized trial. . Zhonghua Er Ke Za Zhi. 2006 Dec; 44(12):913-7.
Molenaers, G., Van Campenhout, A., Fagard, K., De Cat, 3. J., Desloovere, K. (2010) The use of botulinum toxin A in children with cerebral palsy, with a focus on the lower limb. J Child Orthop. 2010 Jun;4(3):183-95. doi: 10.1007/s11832-010-0246-x. Epub 2010 Mar 18.
Ade-Hall, R.A., Moore, A.P., (2000) Botulinum toxin 4. type A in the treatment of lower limb spasticity in cerebral palsy. Cochrane Database Syst Rev. 2000;(2):CD001408.
Horak, F.B., Frank, J., Nutt, J., (1996) Effects of 5. dopamine on postural control in parkinsonian subjects: scaling, set, and tone. J Neurophysiol. 1996 Jun;75(6):2380-96.
Smith, A.D., Dar, M.S., (2006) Mouse cerebellar 6. nicotinic-cholinergic receptor modulation of Delta9-THC ataxia: role of the alpha4beta2 subtype. Brain Res. 2006 Oct 18;1115(1):16-25. Epub 2006 Aug 24.
Lorivel, T., Hilber, P., (2007) Motor effects of delta 9 7. THC in cerebellar Lurcher mutant mice. Behav Brain Res. 2007 Aug 6;181(2):248-53. Epub 2007 Apr 24.
Takakusaki, K., Habaguchi, T., Ohtinata-Sugimoto, 8. J., Saitoh, K., Sakamoto, T., (2003) Basal ganglia efferents to the brainstem centers controlling postural muscle tone and locomotion: a new concept for understanding motor disorders in basal ganglia dysfunction. Neuroscience. 2003;119(1):293-308.
Simonsen, E.B., (2014) Contributions to the 9. understanding of gait control. Dan Med J. 2014 Apr;61(4):B4823.
Kubin, L., Reignier, C., Tojima, H., Taguchi, O., Pack, 10. A.I., Davies, R.O., (1994) Changes in serotonin level in the hypoglossal nucleus region during carbachol-induced atonia. Brain Res. 1994 May 9;645(1-2):291-302.
Funk, G.D., Zwicker, J.D., Selvaratnam, R., Robinson, 11. D.M., (2011) Noradrenergic modulation of hypoglossal motoneuron excitability: developmental and putative state-dependent mechanisms. Arch Ital Biol. 2011 Dec 1;149(4):426-53. doi: 10.4449/aib.v149i4.1271.
Halata, Z., Baumann, K.I., (1999) Sensory nerve 12. endings in the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp 427- 437,1999
Machida, M., (1999) Cause of idiopathic scoliosis.13. Spine (Phila Pa 1976). 1999 Dec 15;24(24):2576-83.
Machida, M., Miyashita, Y., Murai, I., Dubousset, J., 14. Yamada, T., Kimura, J., (1997) Role of serotonin for scoliotic deformity in pinealectomized chicken. Spine (Phila Pa 1976). 1997 Jun 15;22(12):1297-301.
Machida, M., Dubousset, J., Yamada, T., Kimura, 15. J., Saito, M., Shiraishi, T., Yamagishi, M., (2006) Experimental scoliosis in melatonin-deficient
International Journal of Research in Medical and Clinical Sciences 57
Journals Era Publications
C57BL/6J mice without pinealectomy. J Pineal Res. 2006 Aug;41(1):1-7.
Pompeiano, O., Manzoni, D., Miele, F., (2002) Pineal 16. gland hormone and idiopathic scoliosis: possible effect of melatonin on sleep-related postural mechanisms.Arch Ital Biol. 2002 Apr;140(2):129-58.
Locati, F., Fedeli R., (2009) Correlazione tra 17. deglutizione scorretta, secrezione di serotonina e scoliosi in età evolutiva; Tesi Master in Posturologia, Univ. Sapienza Roma, 2009
Tamburro, A., Severino, A., Nastro, S., (2010) 18. Valutazione dei valori urinari di serotonina in ragazzi scoliotici, prima e dopo tre mesi di rieducazione della deglutizione; Tesi Master in Posturologia, Univ. Sapienza, Roma,2010
Ferrante, A., Ferrante, Al., Ferrante, C., (2023) A 19. new contribution to the knowledge of Adolescent Idiopathic Scoliosis (AIS); Vol.8, issue 3; 2023
Ferrante, A., Ferrante, Al., Ferrante, C., (2023) 20. Reflection on Fibromyalgia – A New Interpretation; International Journal of Research in Medical and Clinical Science ; Vol.1, Issue 2, 2023 PP:08-13
Cite this article: Ferrante A., Ferrante Al., Ferrante C. The Physiological Control of Muscle Tone: The Effects of Naso-Palatine Stimulation. International Journal of Research in Medical and Clinical Sciences. 2023;1(2): 53-57.
Copyright: © 2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Reflections on Fibromyalgia – A New Interpretation
International Journal of Research in Medical and Clinical Science
Volume 1, Issue 2, 2023, PP: 08-13
www.journalserapublications.com
Research Article
Reflections on Fibromyalgia – A New Interpretation
Antonio Ferrante1, Alberto Ferrante2, Claudia Ferrante3
1Odontostomatologist, master professor in Posturology University of Pisa, Univ. “Federico II” Naples
2Specialist doctor in Physiatry and rehabilitation, Osteopath
3Physiotherapist
Abstract
Introduction: The problem of fibromyalgia is extremely complex and evaluated in different and discordant ways by the various specialists.
Objective: Our research started from completely different bases, compared to specialized rheumatological studies, but perhaps, the possibility of looking for an explanation starting from a “clean slate”, without any preconception, it allowed us to bring a partly new vision, based on our knowledge and skills, different from rheumatological ones. We wanted to show that many Fibromyalgias find their origin in swallowing dysfunction.
Methods: Our work was based on the use of devices suitable for measuring orofacial muscles (Myometer), muscle tone (surface electromyography), urinalysis to evaluate the catabolites of neuromediators and hormones produced. The results help to understand the mechanisms through which Fybromialgia is created and worsened and indicate a way for its improvement. We evaluated 20 patients with a diagnosis of fibromyalgia, referred to our clinic for problems of the temporomandibular joints and who, according to our treatment method, required the re-education of the swallowing function before resorting to the application of a specific bite for mandibular repositioning. Inclusion criterion was the diagnosis of fibromyalgia. Exclusion criterion: presence of third or fourth degree short frenulum (extremely blocked tongue and frankly ankylotic tongue) which would not have allowed re-education of swallowing without performing a frenulotomy before the start of therapy oral rehabilitation.
Results: After four months of re-education, necessary to rebalance the tongue muscles, improvements in the general tone of the muscles were found in 16 patients. The patients, who had no or minor improvement, still had difficulty managing the muscles of the tongue. Evident improvements were obtained on the ATM symptoms (decrease or disappearance of joint noises), on the headache, with complete disappearance in the patients who had reduced the value of the contraction of the masseters, measured with the Myometer. An improvement in sleep and psychic attitude was also appreciated.
Discussion: From what has been said, it is clear that there is a beneficial effect following the recovery of the stimulation of the naso-palatine receptors. This opens up a new path for the control and disappearance of fibromyalgia.
Conclusion: Among the causes of fibromyalgia, incorrect swallowing plays an important role.
Keywords: Melatonin, Serotonin, Trigeminus Nerve, Incorrect Swallow.
*Corresponding Author: Antonio Ferrante, Odontostomatologist, master professor in Posturology University of Pisa, Univ. “Federico II” Naples
International Journal of Research in Medical and Clinical Sciences
Introduction
We have extracted this definition from a specialist website. Fibromyalgia, also called fibromyalgia syndrome, is the leading cause of widespread pain syndrome, a chronic type condition associated with many other symptoms.
At the time of the visit, the pain is exacerbated if pressure is exerted on specific points and can also make it difficult for the sufferer to move. The causes of the occurrence of fibromyalgia are not yet known. At the moment, experts believe that it can arise due to a combination of genetic, infectious, hormonal factors and also following physical and psychological trauma. In practice there is no certain knowledge in the matter.
The main symptom of fibromyalgia is widespread pain throughout the body, which however can be associated with other symptoms such as asthenia, unsatisfactory night rest, headache more often with tensive characteristics, intestinal disorders such as irritable bowel syndrome (constipation alternating with diarrhea), difficulty concentrating and feeling swollen in the hands and feet (1,2,3,4). When these symptoms occur, those who suffer from it if subjected to a medical investigation do not report damage to joints, muscles or organs.
Fibromyalgia can appear gradually, getting worse over time, or it can arise after a triggering event, such as physical trauma, infection or psychological stress.
In order for the specialist to diagnose fibromyalgia, he must first make sure that the symptoms are not associated with other pathologies, also through blood tests that evaluate the autoimmune picture. Difficulty pinpointing a cause for these symptoms can be associated with and worsen anxiety and depression, which in turn can contribute to worsening chronic pain.
All the specialists find that in addition to the muscle-type symptoms there are other “accompanying” ones that are difficult to explain. In fact, the only reading capable of explaining all the symptoms, including hormonal, intestinal and psychic ones, is the one that derives them from a lack of stimulation of the nasopalatine receptors characteristic of impaired swallowing. We need to clarify some key points. The neurophysiological explanation comes from a research conducted in various animal species by Halata and Baumann (5), who had discovered the presence, at the emergence of the naso-palatine nerve (II trigeminal branch), of the five exteroceptors most present in the human body.
At this point I must explain that the naso-palatine hole (fig.1) (defined Spot in Myofunctional therapy)(6) is considered the point of support of the tongue on the palate during physiological swallowing. In subjects presenting an incorrect swallow, stimulation of the aforementioned receptors is almost always decreased or lacking. Many are the causes of alterations in swallowing mechanics.(7). The numerically most important reason is feeding with artificial methods (8). In breastfeeding the newborn unconsciously learns to swallow with the pressure of the tongue against the palate, compressing the nipple to obtain the squeezing. In bottle feeding, the newborn is forced by the teat to a low tongue position and learns to use only the lingual muscles with a horizontal function, losing the ability to lift the tip of the tongue in contact with the palate. In this case the tongue will become inefficient for swallowing and will be replaced by the buccinator muscles. These are able to help swallowing, but cause problems both on the structure of the jaws and in even distant areas. Other causes are given by birth compressions of the hypoglossal nerve during natural childbirth and anatomical problems such as a very short frenulum and ankylotic tongue (9). If stimulation of the palatine receptors in the dysfunctional patient can only be impeded or diminished, in the patient with ankyloglossia it is completely prevented. This last cause is frequent in the fibromyalgic patient. In fact, the presence of an anatomical impediment to lift the tongue against the palate determines the often absolute absence of trigeminal stimulation with all the consequences.
Figure 1. Nose-palatal hole
Journals Era Publications
Let us now analyze the symptoms of the fibromyalgic patient read in the light of the alteration of the tongue function. Muscle pains are caused by widespread hypertonicity due to a lack of serotonin. This substance is produced by stimulating the second branch of the trigeminal nerve at its emergence on the palate. In previous research we have demonstrated the ability to increase serotonin production up to three times when the receptors are rhythmically stimulated for three months (10,11). Serotonin is also responsible, together with noradrenaline (produced directly by the Locus coeruleus), for the emotional aspect, for controlling anxiety and depression. Palatine receptors are also responsible for the secretion of melatonin. Again ignorance dominates. Melatonin is proposed for sleep problems, but has no direct effect on sleep. Instead, it controls all circadian rhythms, including sleep-wake rhythm. But much more important are the timed control of the production of Cortisol, Leptin and Ghrelin (the substances responsible for hunger and satiety). Thyroid control is also fundamental, as is participation in the control of immunity. It is unbelievable that there are thousands of indexed searches on its functions and that it is instead linked only to sleep. All these symptoms are related to the lack of stimulation of the palate. There are others instead linked to the altered swallowing mechanism. In the correct, physiological function, during the swallowing act, only the group of muscles that make up the tongue is activated and subsequently the pharyngeal and laryngeal muscles contract. This allows food to be ingested with the help of a negative air pressure that is generated in the pharynx. In incorrect swallowing, the tongue is unable to do its job and is replaced by the contraction of the orbicularis labii and buccinators muscles. These muscles allow you to swallow through the generation of a positive air pressure. This means that the food is swallowed together with large amounts of air. The ingested air distances the stomach favoring an increase in the production of hydrochloric acid. Ipeacidity stimulates an increase in peristalsis which has the purpose of removing the acid and pushing it into the intestine. Being produced in excess, not all the acid is neutralized and this causes a series of symptoms. Among the main ones the tendency to the so-called irritable bowel (12), to the alteration of the absorption of various substances among which iron is greatly affected by the substitution of saprophytic bacteria with acidophilic bacterial colonies, capable of sometimes producing toxins and facilitating intestinal ulcers.
We started to take an interest in fibromyalgia because almost all fibromyalgia sufferers come to our office for TMJ problems. By measuring the stomatognathic muscles during the initial visit, especially the lingual activity (Prof. Harold Gelb, one of the world’s leading gnathologists, stated that a jaw cannot be repositioned if the tongue has not been treated), all patients presented, both with the Myometer and with surface electromyography, an evident hypertonia, which is precisely the main sign of fibromyalgia. Patients began with lingual re-education to facilitate subsequent comfortable use of the mandibular positioner. After the first months of rehabilitation of the swallowing function, the patients, when questioned on the persistence or otherwise of the symptoms presented at the first visit, almost always denoted an evident decrease in pain corresponding to the reduction in the hypertone values presented at the beginning of the therapy. Almost all patients had the explanation: “perhaps the improvement is due to the improvement in the weather”. At six months and more the discomfort continued to improve or to disappear completely and the response of the treated subjects was almost invariably; “maybe it wasn’t true fibromyalgia because fibromyalgia is incurable!”
Objective
Our research started from completely different bases, compared to specialized rheumatological studies, but perhaps, the possibility of looking for an explanation starting from a “clean slate”, without any preconception, it allowed us to bring a partly new vision, based on our knowledge and skills, different from rheumatological ones. We wanted to show that many Fibromyalgias find their origin in swallowing dysfunction.
Methods
Our work was based on the use of devices suitable for measuring orofacial muscles (Myometer), muscle tone (surface electromyography), urinalysis to evaluate the catabolites of neuromediators and hormones produced. The results help to understand the mechanisms through which Fybromialgia is created and worsened and indicate a way for its improvement. We evaluated 20 patients with a diagnosis of fibromyalgia, referred to our clinic for problems of the temporomandibular joints and who, according to our treatment method, required the re-education of the swallowing function before resorting to the application of a specific bite for mandibular repositioning. Inclusion criterion was the diagnosis of fibromyalgia. Exclusion criterion: presence of third or fourth degree short frenulum (extremely blocked tongue and frankly ankylotic tongue) which would not have allowed re-education of swallowing without performing a frenulotomy before the start of therapy oral rehabilitation. A group of ten fibromyalgia subjects who did not undergo therapy was the control group.
The initial values of the orofacial muscles (compressive capacity of the lips, anterior lingual thrust, contractile activity of the masseter muscles) were evaluated with a specific device, the Myometer. We reevaluated the masseter muscles with surface electromyography. We analyzed the excretion of a serotonin catabolite 5-hydroxyindoleacetic acid in the urine of patients. Serotonin, as stated above, is produced during physiological swallowing through the stimulation of the trigeminal palatine receptors, We retested the patients in the same way after four months of re-education of the muscles involved in swallowing.
Results
After four months of re-education, necessary to rebalance the tongue muscles, improvements in the general tone of the muscles were found in 16 patients. The patients, who had no or minor improvement, still had difficulty managing the muscles of the tongue.
Evident improvements were obtained on the ATM symptoms (decrease or disappearance of joint noises) 14/20, on the headache 15/20, with complete disappearance in the patients who had reduced the value of the contraction of the masseters whose hypertonicity causes tension headaches (Tab.1), measured with the Myometer, compared to a group of ten fibromyalgia subjects who did not undergo therapy was the control group (Tab.2)
Table 1. Average of Electromyographic changes in four months of spot stimulation through myofunctiona therapy
Table 2. Average of Electromyographic changes in four months In the control group
Discussion
From what has been said, it is clear that there is a beneficial effect following the recovery of the stimulation of the naso-palatine receptors. This opens up a new path for the control and disappearance of fibromyalgia.
Conclusion
Certainly fibromyalgia is a complex and disabling disease that affects countless areas of the body with varied symptoms. It is equally true that the explanations proposed so far make patients feel condemned to “chronic
The results obtained with electromyography (Fig.2,3,4) were similar in each case to the results of the myometer. Improvement in digestive system problems, sleep and psychic attitude was also appreciated.
Figure 2. Emg before and after 4 months
Fig ure 3. Emg head and trunk muscle
Figure 4. Emg after 4 months of Myofunctional stimulation
13 International Journal of Research in Medical and Clinical Sciences
Journals Era Publications
pain”. This new interpretation, based on objective criteria and multidisciplinary skills, allows us to open a window on the possibility that it is in fact a dysfunction that has lasted for years, but which can be resolved or in any case improved by resuming a fundamental function such as correct swallowing.
References
Sarzi-Puttin1 i P, Giorgi V, Marotto D, Atzeni F; Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment; Nat Rev Rheumatol. 2020 Nov;16(11):645-660
Chinn S,2 Caldwell W, Gritsenko K; Fibromyalgia Pathogenesis and Treatment Options Update; Curr Pain Headache Rep. 2016 Apr;20(4):25
Binkiewicz-Glińsk3 a A, Bakuła S, Tomczak H, Landowski J, Ruckemann-Dziurdzińska K, Zaborowska-Sapeta K, IKowalski I, Kiebzak W.: Fibromyalgia Syndrome – a multidisciplinary approach; Psychiatr Pol. 2015;49(4):801-10.
Theoharides4 T C, Tsilioni I, Arbetman L, Panagiotidou S, Stewart J M, Gleason R M, Russell I.J.:Fibromyalgia syndrome in need of effective treatments; J Pharmacol Exp Ther. 2015 Nov;355(2):255-63.
Halata Z, Baumann K I: “Sensory nerve endings in 5 the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp 427-437,1999
Ferrante A: 6 Terapia miofunzionale – dalla deglutizione atipica ai problemi posturali”, Futura Publ. Society, 1997
Ferrante A: La nuova Terapia Miofunzionale; 7 Ed.Centro Terapia Miofunzionale, 2022
Ferrante A, Silvestri R, Montinaro C:The importance 8 of choosing the right feeding aids to maintain breast-feedign after interruption; I.J.O.M.; vol.32,pg. 58, 2006
Ferrante A: Frenulo linguale corto; ed. Centro Terapia 9 miofunzionale.10/2017
Locati F, Fedeli R: 10 Correlazione tra deglutizione scorretta, secrezione di serotonina e scoliosi in età evolutiva. Università La Sapienza, Roma, anno acc. 2008/2009.
Tamburro S, Severino A, Nastro S: Valutazione dei valori 11 urinari di serotonina in ragazzi scoliotici, prima e dopo tre mesi di rieducazione della deglutizione. Università Sapienza, Roma, anno acc. 2009/2010.
Guan Q12 : A Comprehensive Review and update on the pathogenesis of Infiammatory Bowel Disease;.J Immunol Res. 2019 Dec 1;2019:7247238.
Weiss G A, Hennet T13 : Cell Mol Life Sci. 2017 Aug;74(16):2959-2977.
Liu S, Gao J, Zhu M, Liu K, Zhang HL:14 Gut Microbiota and Dysbiosis in Alzheimer’s Disease: Implications for Pathogenesis and Treatment. Mol Neurobiol. 2020 Dec;57(12):5026-504
Han H, Li Y, Fang J, Liu G, Yin J, Li T, Yin Y.: Int J Mol Sci. 15 2018 Mar 27;19(4):995
Cite this article: Antonio Ferrante, Alberto Ferrante, Claudia Ferrante. Reflections on Fibromyalgia – A New Interpretation. International Journal of Research in Medical and Clinical Sciences; 2023; 1(2); 08-13.
Copyright: © 2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
A new contribution to the knowledge of Adolescent Idiopathic Scoliosis (AIS)
A new contribution to the knowledge of Adolescent Idiopathic Scoliosis (AIS)
Antonio Ferrante1, Alberto Ferrante2, Claudia Ferrante3
1 Medico Chirurgo, Spec. in Odontostomatologia, prof. Master in Posturologia clinica Univ. Pisa, Federico II Napoli 2 Medico Chirurgo, spec. in Medicina fisica e riabilitativa , 3 Fisioterapista
Keywords:
Scoliosis, Melatonin, Serotonin, Pineal gland, Trigeminus nerve, Incorrect swallow.
Abstract
Introduction. The problem of idiopathic scoliosis is extremely complex and evaluated in different and discordant ways by the various specialists. All authors agree on one thing: the aethiology of adolescent idiopathic scoliosis still now, after many years of research and studies, is unknown! [1] Theories on AIS’s aethiology have included mechanical, metabolic, hormonal, neuromuscular, growth, and genetic abnormalities. Amongst these, some factors may be epiphenomena rather than the cause itself. [1] Objective. Our research started from completely different bases, compared to specialized orthopedic studies, but perhaps, the possibility of looking for an explanation starting from a “clean slate”, without any preconception, it allowed us to bring a partly new vision, based on our knowledge and skills, different from orthopedic ones. we wanted to show that many scoliosis find their origin in swallowing dysfunction. Methods. Our work was based on the use of devices suitable for measuring orofacial muscles (Myometer), muscle tone (surface electromyography), urinalysis to evaluate the catabolites of neuromediators and hormones produced. The results help to understand the mechanisms through which Scoliosis is created and worsened and indicate a way for its control and often its improvement. WORKING GROUP: N = 40 subjects aged 18-25 years not suffering from diseases of the spine, submitted to postural basic examination and electromyography at rest.
Rescreened with the same parameters after placement of the tongue at the level of the spot Palatine (emergence of the nasal-palatine nerve)
CONTROL GROUP: The same 40 patients constituted the control group, examined after the underlying condition, with different positioning of the tongue (contact with the lower incisors).
The control group has positioned the tongue in different position.
Results study 1 All the subjects, who present muscular imbalances and hypertones at the first examination, rebalanced the values of the various muscles tested (oral, dorsal and paravertebral muscles) as soon as the tongue was placed in contact with the palatine receptors. The positioning of the tongue in different places did not give similar results. Discussion From the analysis of the tests, the tongue shows to have a noticeable effect on the overall posture. This effect is mediated by the change and the rebalancing of the muscular tone through a better functional relationship between the various muscular chains.
Results study 2 The analysis of the values of 5hydroxydolacetic acid, catabolite of serotonin in the urine of 24 hours, allowed to highlight a greater production of serotonin with the exercises of positioning the tongue in contact with the spot. Discussion Studies are confirmed that serotonin deficiency is implicated in the appearance of juvenile idiopathic scoliosis.
Introduction
Many researchers have recognized a multiplicity of ethiological causes [2] giving importance, based on their cultural background, to the visual system, the vestibular system, occlusion, neuromuscular or developmental problems, endocrine disorders, genetic.
The role of serotonin and melatonin in scoliosis is controversial. [3,4,5,6,7,8,9]. In fact, specific receptors for these substances have been found along the entire spinal column. However, no one has analyzed other elements correlated with the alterations of these two substances.
We leave out the general and biochemical mechanisms related to melatonin. Let’s just remember that Melatonin and Serotonin are produced by the pineal gland. Serotonin is produced during the day, Melatonin at night, in the dark and in sleep.
The initial studies of the relationships between the pineal gland is mainly due to the research of Machida and others who created scoliosis in chickens through the ablation of the pineal gland. [10, 11].
Being a gnathologist and orthodontist and having been interested in the rehabilitation of orofacial muscles and swallowing in my treatments for thirty years, I soon realized changes in posture obtained “involuntarily” in patients who practiced myofunctional therapy as a support and prologue to specific oral treatments. (fig.1,2)
Fig 1 Patient before MFT Fig 2 After MFT
For many years I searched for an explanation for what I saw very often: patients improved in orofacial muscular balance, but also, almost always, in postural attitudes and scoliosis [12] during the swallow rehabilitation.
However I could find no explanation. Then, I happened to read a research conducted in various animal species by Halata and Baumann [13], who had discovered the presence, at the emergence of the naso-palatine nerve (II trigeminal branch), of the five exteroceptors most present in the human body.
At this point I must explain that the naso-palatine hole (fig.3,4) (defined Spot in Myofunctional therapy) is considered the point of support of the tongue on the palate during

Fig 3 Palatine hole Fig 4 Nose-palatine Nerve
physiological swallowing. In subjects presenting an incorrect swallow, stimulation of the aforementioned receptors is almost always decreased or lacking. Many are the causes of alterations in swallowing mechanics. [14] The numerically most important reason is feeding with artificial methods. In breastfeeding the newborn unconsciously learns to swallow with the pressure of the tongue against the palate, compressing the nipple to obtain the squeezing. In bottle feeding, the newborn is forced by the teat to a low tongue position and learns to use only the lingual muscles with a horizontal function, losing the ability to lift the tip of the tongue in contact with the palate. In this case the tongue will become inefficient for swallowing and will be replaced by the buccinator muscles. These are able to help swallowing, but cause problems both on the structure of the jaws and in even distant areas. Other causes are given by birth compressions of the hypoglossal nerve during natural childbirth and anatomical problems such as a very short frenulum and ankylotic tongue. If stimulation of the palatine receptors in the dysfunctional patient can only be impeded or diminished, in the patient with ankyloglossia it is completely prevented. I remember that the anatomical alterations of the tongue are genetic and often the patient with ankylotic tongue presents scoliosis [15], but no one has referred to this type of genetics.
About 70% of the cases of patients with scoliosis that belong to my office have alterations in swallowing accompanied by malocclusions and associated muscle imbalances. It is often possible, by measuring the masseters, to understand what is the alteration of tone in the spine and the type of curve that we can find.
For many years we have tried to explain the relationship between swallowing and postural alterations, but only the discovery of the naso-palatine receptors has given an impetus to our research. Being a teacher in many Masters in Posturology I was able to assign theses on topics that are not part of the dentist’s cultural background and expand my knowledge on mouth-brain relationships.
The first thing observed was clear. If the attitude and the curves of the spine improved, it was evident to me that the tone of paravertebral and of the trunk musculature was balancing. Lacking research on the subject, I managed to get my son, graduating in Medicine, assigned a thesis on changes in the tone of the paravertebral muscles and trunk by varying the position of the tongue. [16]
Study design 1
Materials and methodologies
In our research we used Electromyograph Myo-tronics Inc. to measure the stomatognathic and trunk muscles, Myometer, to evaluate the function of the tongue and masseter muscles, Black light lamp and Fluorescein in sepigel 1% to evaluate the lingual dynamics during the swallowing act.
40 subjects were tested, all in good health, aged between 18 and 25 years, both genders, with the only common factor of the presence of an incorrect swallowing and an altered tongue posture evaluated through the use of Fluorescein sepigel 1 %. The examination allowed to evaluate the correctness of the tongue movement during the swallowing act detecting the presence of Fluorescein (visible in the mouth through the Wood’s lamp). Once the fluorescein is applied on the lingual apex and on the upper edges of the zone corresponding to the premolars and the spontaneous swallowing of the patient is done, the areas where the Fluorescein appear are detected. In a physiological environment three small round areas are found on the tongue and on the palate, only on the palatine Spot and in the lateral region of the palate at the level of the premolars. In patients with dysfunction of the swallowing coloured streaks can be found on the tongue and colour deposited in places where the tongue touches the oral structures, that is, between the teeth, against the teeth or even on the inner side of the cheeks. Subjects with a short frenulum, spinal disorders or muscular diseases of any kind were excluded. Three evaluations were carried out: the first one with the tongue in habitual wrong position, the second with the tongue resting on the palate at the level of emergence of naso-palatine nerve, and the third positioning the tongue in a different way (against the lower incisors) assessing through the electromyography any potential changes.
In particular, the use of the surface electromyography for this purpose is recognized by the work of many experts of the spinal column and the scoliotic pathologies [19,20,21,22].
WORKING GROUP: N = 40 subjects aged 18-25 years not suffering from diseases of the spine, submitted to postural basic examination and electromyography at rest.
Rescreened with the same parameters after placement of the tongue at the level of the spot Palatine (emergence of the nasal-palatine nerve)
CONTROL GROUP: The same 40 patients constituted the control group, examined after the underlying condition, with different positioning of the tongue (contact with the lower incisors).
Results
Electromyography
Using a surface electromyography it has been evaluated the activity in rest conditions of certain head and trunk muscles and their modifications following the repositioning of the tongue on the palatine spot. A control test was then carried out assessing the muscular activity by placing the tongue against the lower incisors.
Four pairs of muscles were evaluated:
Masseter, Sternocleidomastoid, trapezius and paraspinal muscles at the level of the third lumbar vertebra.
The recordings were made with patients in a sitting position and without that they were been made aware of what was expected by the outcome of the examination.
Below the reference values for each muscle and the standard deviations that allow defining the degree of activity:
Reference Range Standard deviation
Masseter 1.87 microVolts 1.46
Sternocleidomastoid 1.98 microVolts 1.75
Trapeiius 2.78 microVolts 3.03
Paraspinal L3 1.41 microVolts 1.62
Legenda
LMM – Left masseter muscle
LSC – Left sternocleidomastoid muscle
RSC – Right sternocleidomastoid muscle
RMM – Right masseter muscle
LTP – Left trapezius muscle
LPS – Left paraspinal muscle
RPS – Right paraspinal muscle
MTP – Right trapezius muscle
All the subjects, who present muscular imbalances and hypertones at the first examination, rebalanced the values of the various muscles tested (oral, dorsal and paravertebral muscles) as soon as the tongue was placed in contact with the palatine receptors, denoting an effect of an exquisitely neurological nature involving of the cerebellum which, we recall, receives trigeminal information in the paramedian part and lingual information in the cerebellar worm.
Results
The result of the example (fig. 5,6) is similar to that obtained in the other 39 subjects with minimal variations between the individual muscles. The positioning of the tip of the tongue in contact with the palatine receptors showed a clear and immediate effect in almost all the tested patients.
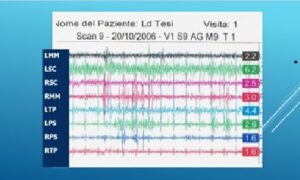
Fig 5 EMG with Tongue in habitual position
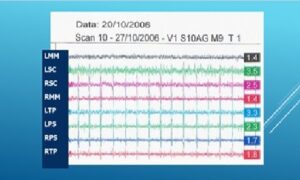
Fig. 6 EMG with Tongue to the Spot
Discussion
From the analysis of the tests, the tongue shows to have a noticeable effect on the overall posture. This effect is mediated by the change and the rebalancing of the muscular tone through a better functional relationship between the various muscular chains. From the tests it clearly appears an improvement in most of tested subjects. The cases that on the other hand showed a worsening or have improved much less than the others by placing the tongue on the Spot denoted a behavior similar to the presence of a short frenulum. The explanation is to be found in the stretching of the lingual muscles in an attempt to lighten the tongue against the palate in the presence of an anatomical impediment.
Conclusions
Research shows that the role of lingual posture and swallowing in people with muscle tension and pain problems cannot be overlooked. A careful analysis of these elements can help in interventions aimed at restoring the well-being of the patient with serious muscle tension otherwise inexplicable such as patients with fibromyalgia, in which knowledge of the damage created by the alteration in swallowing could help to understand the unexplainable symptoms from a physiatric or rheumatological point of view.
Study design 2
Another element was clear to me: if, as Machida et al. stated, adolescent idiopathic scoliosis was due to a deficiency of Melatonin and Serotonin, it could mean that, my patients that improved scoliotic curves during myofunctional treatment, perhaps had defects in the production of these neuromediators and that stimulation of the palatine receptors was able to normalize their production.
To validate this supposition, we carried out two studies by measuring the excretion of 5 hydroxy-indolacetic acid, which is a serotonin catabolite, in the urine during 24 hours.
The research group consisted of sixteen subjects between eight and sixteen years of both sexes (sixteen males and ten females). Ten subjects made up the control group. All presented with scoliosis and alterations in the swallowing mechanism. Subjects in the active group performed three-minute spot tongue placements, three times a day for thirty days.
Results
Working group
– in the male subjects 80,00% increased the serotonin concentration;
– in the female subjects 67,00% increased the serotonin concentration;
Control group
– in the male subjects 29% increased the concentration of serotonin;
– in the female subjects 47% increased the serotonin concentration;
– in the whole sample examined 40% increased their serotonin concentration;
In 70% of scoliotic subjects, low serotonin values improved with palatine stimulation performed for three minutes three times a day. But already the stimulation of the palate for five minutes once a day was able to improve the excretion of this serotonin catabolite. [17, 18] (tab.1,2 ).
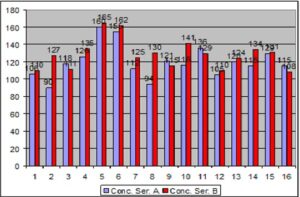
Tab. 1 Concentration in micrograms/24 hours of the initial and final serotonin in the male subjects of the study group. Blue histograms represent the first collection while red histograms indicate the second collection.
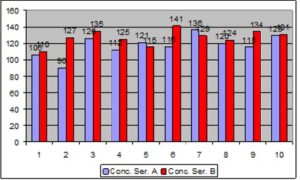
Tab. 2 Concentration in micrograms/24 hours of the initial and final serotonin in the female subjects of the study group. Blue histograms represent the first collection while red histograms indicate the second collection.
The average of increase in subjects with AIS went from 119.88 to 128.56, This data makes us think a lot about the possibility that this Myofunctional Therapy, implemented to restore the correct lingual function, can participate in the regulation of serotonin and muscle rebalancing in subjects with scoliosis.
Changes in the control group were not significant (tab. 3)
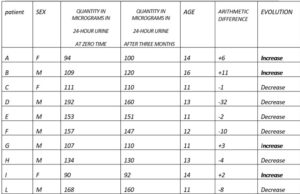
Tab.3 The non-significant changes in concentration in the control group
Conclusion
The analysis of the results that emerged from the studies leads to a single conclusion: probably the appearance and development of idiopathic scoliosis depend more on the muscular imbalance, caused by impaired swallowing, which also affects the spine, than on the lack of melatonin which reflects the poor stimulation of the palatine receptors. The fact that, however, even in the presence of a normal serotonin value, an improvement in its production is obtained by stimulating the palate, tells us that swallowing plays a role in both the onset of scoliosis and its healing.
Bibliography
1 Cheung Kenneth MC, Wang T,Qiu G X, Luk Keith D K: Recent advances in the aetiology of adolescent idiopathic scoliosis, Int Orthop 2008 Dec;32(6):729-
34.doi:1007/s00264-007-0393-y.Epub 2007 Jun 16
2 Girardo M, Bettini N, Dema e, Cervellati S,: The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis (AIS) Eur Spine J. 2011 May;
20(Suppl 1): 68–74.
3 Bagnall KM, Raso VJ, Hill DL, Moreau M, Mahood JK, Jiang H, Russell G, Bering M, Buzzell GR. Melatonin levels in idiopathic scoliosis. 1997;21:1974– 1978. doi: 10.1097/00007632-199609010-00006.
4 Bagnall KM, Raso VJ, Hill DL, Moreau M, Mahood JK, Jiang H, Russell G, Bering M, Buzzell GR. Melatonin levels in idiopathic scoliosis. Diurnal and nocturnal serum melatonin levels in girls with adolescent idiopathic scoliosis. 1996;21:1974–1978. doi: 10.1097/00007632-199609010-00006.
5 Fagan AB, Kennaway DJ, Sutherland AD. Total 24-hour melatonin secretion in adolescent idiopathic scoliosis: a case–control study. 1998;23(1):41–46. doi: 10.1097/00007632-199801010-00009.
6 Hilibrand AS, Blakemore LC, Loder RT, Greenfield ML, Farley FA, Hensinger RN, Hariharan M. The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis. 1996;21:1140–1146. doi: 10.1097/00007632-199605150-00004.
7 Machida M, Dubousset J, Imamura Y, Miyashita Y, Yamada T, Kimura J. Melatonin: a possible role in pathogenesis of adolescent idiopathic scoliosis. 1996;21:1147–1152. doi: 10.1097/00007632-199605150-00005
8 Machida M, Murai H, Miyashita Y, Dubousset J, Yamada T, Kimura J. Pathogenesis of idiopathic scoliosis. 1999;24:1985–1989. doi: 10.1097/00007632- 199910010-00004.
9 Machida M. Causes of idiopathic scoliosis. 1999;24:2576–2583. doi: 10.1097/00007632-199912150-00004
10 Machida M, Dubousset J, Imamura Y, Iwaya T, Yamada T, Kimura J. Role of melatonin deficiency in the development of scoliosis in pinealectomised chickens. J Bone Joint Surg (Br) 1995;77-B:134–138.
11 Machida M, Dubousset J, Imamura Y, Iwaya T, Yamada T, Kimura J. An experimental study in chickens for the pathogenesis of idiopathic scoliosis. 1993;18:1609–1615. doi: 10.1097/00007632-199309000-00007.
12 Ferrante A, Reed-Knight E, Bello A, Comentale P. Variazioni posturali conseguenti a cambiamento della posizione linguale ed a trattamento mio
funzionale; Ortognatodonzia italiana, vol. 11, 3 -2002
13 Halata Z., Baumann K.I.: “Sensory nerve endings in the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp
427-437,1999
14 Ferrante A, Terapia miofunzionale, dalla deglutizione atipica ai problemi posturali”, Futura Publ. Society, 1997
15 Ferrante A. Frenulo linguale corto. Centro Terapia miofunzionale.10/2017
16 Ferrante Alberto. Modificazioni posturali secondarie alla variazione di funzione di alcuni muscoli del capo e del collo. Seconda Università di Napoli. Anno
acc. 2005/2006
17 Locati F. Fedeli R. Correlazione tra deglutizione scorretta, secrezione di serotonina e scoliosi in età evolutiva. Università La Sapienza, Roma, anno acc.
2008/2009.
18 Tamburro S., Severino A., Nastro S.,Valutazione dei valori urinari di serotonina in ragazzi scoliotici, prima e dopo tre mesi di rieducazione della
deglutizione. Università Sapienza, Roma, anno acc. 2009/2010.
19 Avikainen VJ, Rezasoltani A, Kauhanen HA,:”Asymmetry of paraspinal EMG-time characteristics in idiopathic scoliosis”. J Spinal Disord. 1999
Feb;12(1):61-7.
20 Cheung J, Halbertsma JP, Veldhuizen AG, Sluiter WJ, Mauritz NM, Cool JC, Van Horn JR,: “A preliminary study on electromyographic analysis
paraspinal musculature in idiopathic scoliosis”. Eur Spine J. 2005 Mar;14(2):130-7. Epub 2004 Sep 11.
21 Gaudreault N, Arsenault AB, Lariviere C, De Serres SJ, Rivard CH: “Assessment of the paraspinal muscles of subjects presenting an idiopathic scoliosis: an
EMG pilot study”.BMC Musculoskelet. Disord. 2005 Mar 10;6:14.
22 Grassme R,Arnold D, Anders Ch, van Dijk JP, Stegeman DF, Linss W, Bradl I, Shumann NP, Sholle HCh: “Improved evaluation of back muscle SEMG
characteristics by modelling”. Pathophysiology. 2005 Dec;12(4):307-12. Epub 2005 Oct 25.
Dott. Antonio Ferrante
I° traversa Luigi Angrisani, 23
84014 Nocera Inferiore – Sa, Italia
e-mail dott.antonioferrante@gmail.com
The importance of proper trigeminal information in cases of difficulties to become pregnant
Giorn. It. Ost. Gin. Vol. XXXVIII , n.3
Maggio-Giugno, 2016
The importance of proper trigeminal information in cases of difficulties to become pregnant
L’importanza della corretta informazione trigeminale in casi di difficoltà ad iniziare una gravidanza
Antonio Ferrante1, Claudia Ferrante2
1 Adjunct professor in the Master “Clinic Posturology” University of Pisa, University “ Federico II” of NeaplesCoordinator Master “Myofunctional Therapy in Posturology” , University “Sapienza” of Rome,2 Physical therapist, Myofunctional Therapist
Abstract:
The present multiple Case Report aims at constructing a new hypothesis on the difficulty to get pregnant as a potential neurological problem due to a wrong swallow. The correct swallow stimulates trigeminal neuro-receptors of Naso-palatal nerve. This stimulation, through the intervention of Locus Coeruleus, produces serotonin and melatonin in the pineal gland. The reduced production of melatonin, caused by an alteration of swallowing, allows the prolactin’s increase with its negative effects on the outbreak of the ovarian follicles. The rehabilitation of swallowing clearly lowers the production of prolactin and normalizes the functionality of the ovaries allowing conception.
Key words:
Incorrect swallow, Trigeminus, Melatonin, Prolactin, Ovarian Follicles.
A new hypothesis to explain the mechanism that may be involved in the genesis of sleep bruxism (SB)
Articolo originale
Gazzetta Medica Italiana – Archivio per le Scienze Mediche 2021
September; 180(9):399-403
A new hypothesis to explain the mechanism that may be involved in the genesis of sleep bruxism (SB)
Dott. Antonio Ferrante
Docente Master ”Posturologia clinica” Univ. Pisa, Napoli
Autore di contatto: dott. Antonio Ferrante I trav. Luigi Angrisani, 23 84014 Nocera Inferiore (Sa) Italia e-mail dott.antonioferrante@gmail.com
Abstract
Objective: The present study aims at constructing a new hypothesis on bruxism’s potential neurological etiology. Bruxism is not regarded a parafunction or stress reaction but a non-physiological mechanism deployed by patients suffering from incorrect swallow and functional disorders of the trigeminal stimulation in order to support the memorizing of information during sleep and the attention span during the day. Methods: The study was conducted on 80 patients of both genders aged 20—34 years. All were suffering from impaired swallowing. The patients were randomized and clustered in two groups of each 40 persons. The first group’s patients (Group A) underwent myofunctional therapy according to Garliner (modified by Ferrante) for 3 months. Patients clustered in the second group were further divided into two groups of each 20 people. Twenty individuals (Group B1) did not receive any treatment and were simply monitored for bruxism; the remaining 20 patients (Group B2) used “Bite Strips” to reduce parafunctional activities. Inclusion criteria: Patients with night bruxism. Exclusion criteria: Patients with congenital or acquired craniofacial abnormalities, genetic syndromes, neurologic disorders, and psychiatric disorders. Patients taking medicines. Patients with short frenum or tongue tie. Results: in the first group, 34 patients (85% ) stopped bruxism in three months. Conclusion: The new hypothesis may be right.
Key words: bruxism, sleep, incorrect swallow, trigeminus, memory
VARIAZIONI POSTURALI CONSEGUENTI A CAMBIAMENTO DELLA POSIZIONE LINGUALE ED A TRATTAMENTO MIOFUNZIONALE
Dott. Antonio Ferrante, odontostomatologo, libero professionista
Dott. Estelle Reed-Knight, Bc. in Education, Consulente motivazionale
Dott. Antonio Bello, odontostomatologo, dirigente sanitario ASL Sa.1
Dott. Pasquale Comentale, odontoiatra libero professionista
Riassunto
Nel presente articolo viene illustrata la capacità della lingua di influenzare l’assetto spaziale dell’individuo visualizzata su strumenti di analisi posturale, quali lo scoliosometro ed il baropodometro. Si cerca inoltre di spiegare i motivi di tali cambiamenti e si mette in guardia l’ortodontista dall’intraprendere terapie che, pur tecnicamente corrette e rispettose della biomeccanica, manchino della dovuta attenzione per la patogenesi delle anomalie dento- scheletriche che ci si trova a trattare e, durante il trattamento, per lo spazio vitale linguale, indispensabile perché la lingua possa esplicare tutte le sue azioni che, alla luce delle ultime scoperte, non si limitano alle sole fonazione e deglutizione, ma vanno ben oltre, come nell’articolo si cerca di puntualizzare.
Che la lingua possa essere considerata uno dei muscoli principali dell’organismo è un concetto nuovo per la maggioranza dei medici, ed ancor più per gli odontoiatri che, non ostante abbiano continuamente avanti agli occhi una bocca aperta , nella quale la lingua fa bella mostra di sé, il più delle volte non la considerano che un ingombro, un intralcio al proprio lavoro, un ostacolo che impedisce di poter osservare liberamente i denti da valutare o da trattare.
La mancanza di attenzione a quello che succede di continuo nella cavità orale, a volte la mancanza di conoscenza dei meccanismi fisiologici di funzionamento dell’apparato stomatognatico nel suo complesso (ossa, denti, articolazioni temporo-mandibolari, muscoli) (5,15,16,23,27,29) sono alla base di questo paradossale fenomeno per il quale tutto l’apparato stomatognatico viene ridotto esclusivamente alla componente dentaria o osteo-dentaria.
Questo atteggiamento, e specialmente l’ignoranza, ai giorni nostri non sono più ammissibili, soprattutto in tempi in cui le controversie legali con i pazienti sono divenute ormai frequenti, almeno per quei medici che non hanno un occhio continuo all’aggiornamento professionale e che pensano che le cose apprese venti anni fa possano andare bene ancora oggi. Purtroppo non è così ed un bravo medico degli anni settanta è destinato ad essere un incompetente nel duemila ormai iniziato.
Tutto questo preambolo è stato fatto al solo scopo di mettere in risalto che la posizione della lingua è cambiata nella scala di ciò che è importante per la salute. E l’aumento di importanza agli occhi del professionista è stato determinato da un cambiamento di posizione fisica della lingua all’interno della cavità orale. In un osservatore superficiale, questa osservazione può determinare una risata, ma, a pensarci bene, rispetto a cinquanta anni fa, la postura linguale si è molto modificata, adeguandosi allo stile di vita moderno. Continuamente ci viene ripetuto dai nostri pazienti: “..ma cinquanta anni fa non c’erano tante malocclusioni “ e noi per anni abbiamo risposto che”… forse non c’era la cura che abbiamo oggi delle nostre bocche…”. La nostra risposta è in piccola parte giusta, ma in gran parte sbagliata ; cinquanta anni fa non c’era una metodica di allattamento artificiale così comune in ogni ambiente sociale. Già nel 1951 W.B. Straub, aveva riconosciuto l’allattamento con il biberon responsabile principale delle problematiche associate alla deglutizione scorretta (30,31). Ma addirittura risalgono agli inizi del novecento gli studi sulla importanza della muscolatura orale e periorale per il corretto sviluppo del massiccio facciale ed, ancor più importanti, quelli effettuati sulla postura linguale dal medico e dentista francese Pierre Robin, autore del libro “La glossoptose” (28), nel quale la postura linguale scorretta era messa in relazione, con uno studio per quei tempi eccezionale ed avveniristico, con patologie coinvolgenti l’intero organismo.
C’e da chiedersi come possa essere stato gettato nel dimenticatoio per quasi un secolo un patrimonio di rilievi e conoscenze così importante.
Quello che oggi quindi sbandieriamo ai quattro venti e con tanta energia non è niente di nuovo; oggi abbiamo soltanto, grazie alla tecnologia, la possibilità di provare tante asserzioni fondate, in precedenza, sull’intuito e sulla interpretazione di segni clinici.
Per capire bene il meccanismo attraverso il quale la postura linguale corretta ed un equilibrio ritrovato della muscolatura oro-facciale possano avere l’effetto sull’apparato stomato-gnatico, ma anche ricondurre il corpo ad una relazione spaziale ideale (2,6,7,), bisogna tenere presente i comportamenti delle strutture muscolari e le interazioni neuro-muscolari intercorrenti tra le varie regioni anatomiche dell’organismo.
Come ortopedici e fisiatri ben sanno, i nostri muscoli non si muovono come elementi singoli, ma si contraggono per schemi di funzionamento ben definiti, rispondenti al principio della attivazione-deattivazione, che contradistingue il rapporto tra agonisti ed antagonisti, sempre controllati con finezza dalle strutture specializzate encefaliche e cerebellari (10,35). I muscoli quindi si attivano in maniera prestabilita, con il coinvolgimento specifico di gruppi muscolari, collegati tra loro dalle fasce, e presentanti una similarità di tono. Queste corsie fasciali preferenziali che accomunano la funzione contrattile dei vari muscoli danno luogo alle cosiddette “catene muscolari”.(3)
Varie scuole hanno individuato diversi tipi di catena, ma la cosa interessante è che tutti sono concordi nel riconoscere la muscolatura coinvolta nella deglutizione come un elemento fondamentale di varie catene e punto di passaggio tra una catena muscolare e l’altra.
Si rende così evidente come una postura linguale scorretta possa avere influenza sulla statica dell’intero organismo fino ad influenzare l’appoggio plantare (1,18), con l’interessamento di tutte le strutture intermedie tra questi estremi. Oltre che con un meccanismo diretto, la lingua influisce sulla postura anche attraverso un meccanismo per così dire indiretto, mediato dalla posizione spaziale della mandibola, che risente dei danni causati dalla malfunzione muscolare a livello del palato e dell’occlusione in genere.(5,14,15,17,20 )
Nel nostro Centro per la ricerca in ambito miofunzionale, stiamo portando avanti vari studi, che permetteranno di considerare la lingua ancora più importante di quanto lo può essere ora, ed i risultati fin qui ottenuti sono sempre più incoraggianti.
Per la rapidità con cui si possono ottenere risultati apprezzabili dal punto di vista posturale, spesso più rapidi di quelli riscontrabili a livello orale e di carattere ortodontico, può essere preso in considerazione un meccanismo di riattivazione muscolare ed ancor più un miglioramento di tipo osteopatico.
Mentre per quanto riguarda il riguadagno di un equilibrio muscolare non c’è molto da chiarire, può essere opportuno spiegare il concetto di recupero osteopatico. Le conoscenze generali infatti, su che cosa sia l’Osteopatia e quali siano i suoi principi e meccanismi, sono argomenti in Italia ancora sconosciuti ai più, se non addirittura bollati come fisioterapia, chiropratica o peggio come ciarlataneria e forse “stregoneria”.
E’ opportuno pertanto spiegare, a chi ne è all’oscuro, le basi della scienza osteopatica.
L’osteopatia, come la intendiamo ai nostri giorni, è nata negli anni trenta per opera del dottor W.G. Sutherland, allievo diretto di A. T. Steel, colui che per primo aveva individuato il ruolo delle fasce muscolari nel funzionamento dell’organismo.(22,33,35)
Il dott. Sutherland, studiando l’anatomia di un cranio, si rese conto della presenza di smussature sui margini dell’osso temporale che presupponevano la possibilità di movimento. Da questa osservazione scaturirono studi e ricerche anche universitarie che hanno portato negli anni all’accertamento di movimenti ritmici del cranio nel numero di 10/14 al minuto, riscontrati anche in soggetti di età avanzata e denominati “Respirazione Cranica Primaria”(9,34), per indicarne la somiglianza e la primarietà temporale rispetto alla respirazione polmonare. Attualmente negli Stati Uniti vi sono ben diciotto università che rilasciano il diploma di laurea in Medicina Osteopatica e molti sono i paesi in cui le università formano medici osteopati.
Il ritmico espandersi e contrarsi della cavità cranica è responsabile del deflusso del liquido cefalorachidiano verso le guaine dei nervi più periferici ed è determinato, in primo luogo, dalla capacità contrattile dei dieci miliardi di cellule di nevroglia e dalla elasticità delle membrane meningee, specialmente della dura-madre. L’espansione, in ultima analisi, è la conseguenza della secrezione del liquido cefalorachidiano da parte ventricoli cerebrali; lo stiramento di recettori posti all’interno della sutura interparietale inibisce la produzione del liquor mentre l’elasticità della duramadre dà luogo alla contrazione cranica che si accompagna alla spremitura del liquor versi i nervi periferici e al suo riassorbimento da parte dei villi subaracnoidei.
Tutte le fasce dell’organismo possono essere considerate espansioni della duramadre a causa della continuità fisica ed embriologica esistente tra queste strutture; ciò rende conto dei problemi che si creano ogni qualvolta il meccanismo respiratorio cranico è perturbato.
La lingua è un elemento fondamentale per la promozione ed il mantenimento di questo movimento, il cui cessare o modificarsi ha un effetto sul funzionamento delle fasce muscolari dell’intero organismo. Il motivo di questa importanza è dovuto alla inserzione di un muscolo linguale, lo Stiloglosso, alla apofisi stiloide dell‘osso temporale, quindi sulla base cranica. La deglitizione corretta , quella cioè effettuata con attivazione dello Stiloglosso(7), imprime trazioni ritmiche alla base cranica promuovendone il movimento; la deglutizione scorretta, nella quale vengono attivati altri muscoli tra i quali importantissimi i Buccinatori ed il Genioglosso (24) , non è invece in grado di stimolare tale movimento o, addirittura, ne impedisce il normale espletamento.
Comunque, qualunque sia il meccanismo responsabile delle modificazioni, sono state osservate costantemente, salvo poche eccezioni, variazioni della statica posturale soprattutto nell’esame laterale, evidenziate chiaramente sullo scoliosometro.
Questo accade probabilmente perché le modificazioni della postura linguale determinate dal trattamento miofunzionale, determinano il cambiamento della posizione antero-posteriore della mandibola (15), che può essere considerata il nostro bilanciere organico, cioè quello strumento che determina il nostro assetto spaziale.
Il motivo per il quale le variazioni posturali in proiezione frontale sono meno frequenti è presto spiegato: la postura frontale, come quella in lateralità, è in parte determinata dalla posizione mandibolare. Nei pazienti che presentano deglutizione scorretta, la mancanza di sostegno del palato da parte della lingua e la pressione esercitata dalle guance durante l’atto deglutitorio, determinano una diminuzione del diametro trasverso palatino (7).( Quando quest’ultima si accompagna ad un morso crociato monolaterale, la posizione mandibolare è obbligata, per cui permane uno sbilanciamento nella tensione dei due masseteri e temporali in particolare, che provoca, attraverso il coinvolgimento di tutta una serie di muscoli funzionalmente correlati, il mantenimento dello squilibrio posturale . Nei casi in cui la rieducazione determina una correzione del morso (avviene in circa il dieci per cento dei casi), o quando viene ripristinata la correttezza del morso con mezzi ortodontici, vi è comunque il miglioramento auspicato. Lo stesso ripristino della norma posturale si ottiene quando la lingua non abbia determinato una ristrettezza anatomica del palato, ma soltanto lo squilibrio della muscolatura elevatrice della mandibola. Ultime ricerche condotte presso il reparto di Anatomia funzionale dell’Università di Amburgo (19) probabilmente hanno contribuito ad una spiegazione risolutiva di quello che ogni giorno riscontriamo nel nostro lavoro. Già durante la prima visita, posizionando la lingua allo spot, con grande costanza riscontriamo miglioramenti della postura globale (fig.1,2) e dell’appoggio plantare (fig. 3,4) con correzione di atteggiamenti francamente patologici a carico del rachide e dei piedi. Per anni abbiamo cercato una spiegazione a quello che vedevamo, chiedendoci come poteva il posizionamento della lingua allo spot (il punto neutro della postura linguale, situato tra la papilla interdentale e le rughe palatine(fig.5)) determinare un così repentino cambiamento in distretti corporei anche distanti. I colleghi tedeschi hanno trovato, senza darsi una spiegazione, la presenza di ben cinque tipi di esocettori (o esterocettori), cioè dei recettori usati dall’organismo per informare il sistema nervoso centrale sulle tensioni muscolari e quindi sui cambiamenti posturali, in grandissima quantità nel centimetro quadrato compreso proprio tra la papilla interincisiva e le rughe palatine, vale a dire proprio sullo spot linguale. E’ stata la spiegazione che attendevamo da tempo; finalmente c’è una prova che la lingua esercita una funzione di regolazione posturale indispensabile; ad ogni deglutizione infatti il paziente che ingoia correttamente riprogramma la funzione della muscolatura posturale stimolando con la pressione linguale la risposta nervosa, cosa che non avviene in presenza di una deglutizione scorretta, che non porta la lingua a contatto dello spot.
Gli effetti del cambiamento di funzione della lingua sono evidenziati in genere da miglioramenti delle curve rachidee, specialmente apprezzabili con il recupero della fisiologica lordosi cervicale che spesso risulta persa nei pazienti con atteggiamenti linguali scorretti, ma anche le altre curve fisiologiche subiscono un rimodellamento con diminuzione dell’iperlordosi lombare (fig.6,7) ed apertura e simmetrizzazione a livello delle spalle in special modo e con la scomparsa di atteggiamenti scoliotici, quando ,come accennato sopra, sono state eliminate le cause di squilibrio di masseteri e temporali determinate dalla presenza di un morso crociato.
A livello dell’appoggio plantare i cambiamenti più immediati sono costituiti da una diminuzione del carico sull’avampiede , quasi sempre presente nel paziente con deglutizione scorretta, soprattutto in presenza di un frenulo corto, e nel bilanciamento del carico tra i due piedi con un miglioramento del baricentro corporeo. Spesso si assiste alla scomparsa di un piede piatto di grado anche elevato e molto frequentemente alla scomparsa del piede cavo, questo addirittura evidente a volte durante la prima visita, al momento del posizionamento corretto della lingua.(fig.8-9)
Tutti questi cambiamenti dovrebbero essere di monito a quanti si interessano del trattamento dei problemi di appoggio del piede o dei vizi della statica della colonna, per evitare il trattamento di casi che trovano la propria genesi nella disfunzione orofacciale e che, trattati in maniera tradizionale, a mezzo di plantari o di busti, verrebbero soltanto ostacolati nella guarigione, contribuendo a rendere un difetto inizialmente funzionale, alla fine organico.
Dovrebbero essere un avvertimento, d’altra parte, per quanti si interessano di ortodonzia, a non limitare il proprio intervento alle strutture osteo-dentarie, ma anzi uno stimolo a controllare in una maniera più completa i rapporti di causa-effetto determinati dalla malfunzione muscolare oro-facciale sia per quanto riguarda la genesi della patologia ortodontica che per quella di carattere apparentemente ortopedico o fisiatrico; questo al fine di non rendersi responsabili, stabilizzando una occlusione non desiderata dalla muscolatura del soggetto in cura, della permanenza di una disfunzione posturale altrimenti facilmente recuperabile. Oltre tutto, rieducando la muscolatura prima di un trattamento ortodontico, ricaveranno molteplici soddisfazioni per la velocizzazione naturale del trattamento stesso, per la minore necessità di contenzione, per il minore rischio di riassorbimenti radicolari. Basta pensare alla maggior facilità di espansione palatina che si potrà realizzare quando meccanismo ortodontico e muscolatura lavoreranno nella stessa direzione (ricordiamo che la ristrettezza del palato è determinata in primo luogo dalla pressione esercitata dai m. buccinatori durante la deglutizione, pressione che deve essere vinta dall’apparecchio perché possa esercitare la sua funzione e che per questo necessita di applicazioni di forze di gran lunga maggiori di quelle utilizzabili quando le guance, durante la deglutizione sono immobili, e quando la lingua esercita il suo fisiologico movimento comprimendosi contro il palato.(fig.10)
E’ auspicabile quindi che in ogni studio ortodontico possa essere presente l’attrezzatura minima per un controllo posturale e della dinamica deglutitoria per ottimizzare al massimo le possibilità di guarigione del paziente.
Materiali e metodi
Nel presente lavoro sono stati analizzati 415 pazienti di età comprese tra i 6 ed i 61 anni, venuti alla nostra osservazione per patologie legate all’apparato stomatognatico ( in primo luogo pazienti ortodontici 53 %, ma anche pazienti parodontopatici 12 %, pazienti gnatologici 22 %, pazienti con problematiche respiratorie inviatici da colleghi Otorino e Pediatri (pazienti nei quali, con l’esclusione di un caso, abbiamo sempre riscontrato una deglutizione scorretta alla base del problema respiratorio e dei correlati problemi di carattere ortodontico) 11% ; un altro gruppo di pazienti si sono rivolti a noi per problematiche esclusivamente posturali (dolori nei vari distretti vertebrali, recidive di ernie discali, cefalee e cervicalgie muscolo-tensive) 2%.
Tutti i pazienti sono stati valutati sulla pedana stabilometrica ( baropodometro elettronico Physical Support Italia) e sullo scoliosometro (analizzatore posturale Kinesport) nelle condizioni di base e posizionando la lingua allo Spot.
Nessuno dei pazienti è stato informato di ciò che si voleva verificare, ed il risultato delle nostre osservazioni è stato discusso con il paziente o con i genitori soltanto dopo la raccolta di tutta la documentazione.
Si è preferito non fare assolutamente muovere il paziente dalla sua posizione iniziale (anche sapendo che farlo deambulare dopo il posizionamento linguale allo spot avrebbe ottenuto un decondizionamento neuro-posturale maggiore ) perché non volevamo che si potesse obiettare che le nostre valutazioni erano alterate dal riposizionamento del paziente sullo strumento di controllo e che i nostri miglioramenti erano soltanto legati al caso. Si è infine affidato ad una persona differente dall’operatore della analisi il compito di indicare al paziente il punto del palato in cui posizionare la lingua.
Si è analizzato anche un gruppo di controllo composto da 22 persone con deglutizione corretta ed assenza di evidenti anomalie occlusali. Sarebbe stato auspicabile un gruppo di controllo di maggiore entità numerica, ma è risultato oltremodo difficile reperire persone con deglutizione non alterata.
Risultati
Analizzeremo per primi i risultati ottenuti sul baropodometro
I pazienti esaminati erano accomunati dal presentare una deglutizione scorretta. Nel presente lavoro non abbiamo ritenuto di distinguere gli otto tipi di deglutizione riconosciuti dal prof. Daniel Garliner pur avendo evidenziato piccole differenze tra i vari tipi, probabilmente valutati in una prossima ricerca.
Per le valutazioni sul baropodometro sono stati presi in considerazione:
– La distribuzione del carico tra avampiede e retropiede (in percentuale)
– La superficie dell’appoggio plantare espressa (in cm. quadrati)
– La distribuzione del carico tra piede destro e sinistro (in chilogrammi e percentualmente)
Per quanto riguarda il rapporto di carico tra avampiede e retropiede, che dovrebbe nell’ideale essere di 40% anteriormente e 60% posteriormente, abbiamo considerato normali valori compresi tra il 57 e 63 % per il carico sul retropiede. Si è riscontrato che soltanto il 10,1 % presentava inizialmente un rapporto corretto, pur essendo presenti comunque piccole variazioni tra piede destro e sinistro.
Posizionando la lingua allo spot si sono ottenuti i seguenti risultati:
Rapporto a/r (avampiede-retropiede)
– Peggioramento in121 pazienti, pari al 29,1%
– Valori invariati in 107 pazienti, pari al 25,8 %
– Miglioramento in 187 pazienti 45,1 %
Superficie di appoggio piede destro/piede sinistro
– Peggioramento in 111 pazienti, pari al 26,7 %
– Valori invariati in 72 pazienti, pari al 17,3 %
– Miglioramento in 233 pazienti, pari al 56 %
Distribuzione del carico tra piede destro e sinistro
– Peggioramento in 60 pazienti, pari al 14,4 %
– Valori invariati in 84 pazienti, pari al 20,2 %
– Miglioramento in 271 pazienti, pari al 65,4 %
Nel gruppo di controllo, essendo la lingua già allo spot alla prima misurazione, abbiamo valutato solo i valori di base. Essi sono risultati abbastanza vicini alla norma, riscontrandosi, per quanto riguarda il rapporto a/r valori alterati, compresi comunque entro lo scarto di 5 punti percentuali (per il retropiede un carico tra il 55 e 65% ) in 6 pazienti; anche la differenza di superficie di appoggio è risultata abbastanza omogenea, con variazioni di misura non superiore al 3 %. Il peso corporeo era infine distribuito adeguatamente e la differenza non superava il 2% (49% su un piede, 51 sull’altro).
Sullo scoliosometro le variazioni sono state oltremodo evidenti.
I pazienti del gruppo controllo sia in visione frontale che laterale hanno presentato un atteggiamento posturale corretto. Nell’esame laterale i punti di repere erano allineati in 17 pazienti, mentre nei 5 rimanenti si riscontrava una distanza del trago dalla verticale di Barrè non superiore ai due centimetri con un leggero avanzamento del capo in due soggetti dovuto alla necessità di correzione con lenti, operata la quale vi era un recupero della verticalità.
Nell’esame frontale i pazienti presentavano allineamento della colonna e del livello delle spalle ad eccezione di un soggetto in permuta dentaria con mancanza degli elementi dentari 85-84 non ancora sostituiti dai permanenti.
I 415 pazienti oggetto della ricerca, analizzati con la solita metodica del test in atteggiamento naturale seguito da quello con la lingua allo spot, all’analisi laterale hanno mostrato posizioni al di fuori della verticale di Barrè in 351 casi (329 erano in avanti rispetto alla verticale, 22 in dietro). All’esame frontale 324 presentavano spalle non allineate orizzontalmente e, alla visione riflessa dallo specchio posto superiormente allo scoliosometro, 263 mostravano rotazioni sull’asse della colonna e 254 atteggiamento delle spalle in chiusura (spalle ruotate in avanti). Inoltre 311 soggetti presentavano uno spostamento latero-laterale del busto con spostamento del capo rispetto alla verticale. Soltanto 6 pazienti mostravano una evidente deviazione laterale del bacino rispetto alla norma.
Posizionando la lingua allo spot si sono ottenuti i seguenti risultati:
Sul piano sagittale
– Peggioramento (allontanamento dalla verticale) in 12 casi, il 2,9% , 10 dei quali presentavano un frenulo linguale corto.
– Nessuna variazione in 44 casi, pari al 10,6%
– Miglioramento in 359 pazienti, cioè l’ 86,5%, 169 dei quali avevano un recupero totale della verticalità.
Sul piano frontale
– Peggioramento in 2 casi , pari allo 0,5 %
– Nessuna variazione in 89 casi, pari al 21,4 %
– Miglioramento in 324 soggetti, cioè nel 78,5 %, dei quali 112 recuperavano totalmente.
Conclusioni
Dalle misurazioni effettuate risulta evidente l’influenza della postura linguale nella determinazione dell’assetto spaziale corporeo. Una postura linguale bassa si è mostrata causa costante di atteggiamenti posturali scorretti sia alla valutazione sullo scoliosometro che sul baropodometro. La maggior parte dei pazienti analizzati hanno mostrato un atteggiamento anteriorizzato di tutto il corpo, ed hanno evidenziato un raddrizzamento sulla verticale di Barrè con miglioramenti fino al recupero completo della verticalità già durante la prima visita, con il puntamento della lingua allo spot. Ancora più evidente è stato il miglioramento dopo i primi mesi di rieducazione miofunzionale. Un riscontro pressocchè costante è stato quello di una normalizzazione delle curve corporee con diminuzione della iperlordosi lombare che è altrimenti estremamente frequente.
All’analisi sul baropodometro, al riposizionamento linguale è immediatamente seguito un miglioramento del carico sui piedi con spostamento del baricentro corporeo e molto spesso con cambiamenti eclatanti della superficie di appoggio che è risultata più uniforme. A volte c’è stato un cambiamento istantaneo da piedi cavi a piedi normali (ciò è estremamente importante per il fatto che tanti pazienti, se visitati da un ortopedico non accurato, potrebbero venir trattati con plantari che avrebbero la capacità di impedire un eventuale miglioramento spontaneo dell’appoggio, costringendo il piede a permanere nel suo difetto. Per quanto riguarda il piede piatto i miglioramenti, con ritorno ad un aspetto fisiologico sono abbastanza costanti, ma più lenti, ottenendosi miglioramenti evidenti solo dopo qualche mese di terapia, probabilmente perché legati ad un aumento di tono generale della muscolatura responsabile del mantenimento delle arcate plantari, aumento di tono che richiede un certo lasso di tempo per instaurarsi.
Un caso un po’ a parte è costituito dai pazienti con frenulo corto: in questi spesso il posizionamento della lingua allo spot risulta difficoltoso e, comunque, avviene con uno sforzo muscolare che si riflette, soprattutto sul baropodometro, su atteggiamenti podalici non sempre prevedibili. In questi pazienti si torna alla norma dopo la frenulotomia; addirittura potrebbe in alcuni casi essere proprio l’esame baropodometrico a valutare se il paziente deve necessariamente essere sottoposto alla incisione del frenulo o ci si può invece affidare alla fisioterapia per ottenerne l’allungamento e la diminuzione della tensione.
Da quanto sopra esposto risulta chiara l’importanza di un approccio globale al paziente ortodontico per poter minimizzare il rischio che patologie che possono trovare una causa nella disfunzione della muscolatura oro-facciale o nella malocclusione vengano trattate da altri specialisti con esiti incerti e non lavorando sulla causa , ma sugli effetti del problema.
BIBLIOGRAFIA
1) BALERCIA L., BALERCIA P.,”Fisiopatologia della deglutizione. Relazioni tra
occlusione e postura”, Dentista mod. 1,57-83,1993
2) BONDI M., “Mioterapia orofacciale craniocervicale”, Masson ed., 1991
3) BOUSQUET L.;”Le catene muscolari”,vol.I, Marrapese ed. 1994
4) CASELLA G., CORTESI R., GHILARDI L., LAZZARI E.:”Approccio globale alla stabilità in Ortodonzia”,Convegno Naz. S.I.D.O. Firenze, 1990
5) COULY G.:” La lingua apparecchio naturale di ortopedia dento-facciale nel bene e
nel male”. Mondo ortodontico, vol.XIV,6/1989
6) FERRANTE A.,”La deglutizione atipica”, Il dentista Moderno., 2,227-239, 1995
7) FERRANTE A., “Terapia miofunzionale, dalla deglutizione atipica ai problemi
posturali”, Futura Publ. Society, 1997
8) FERRANTE A., REED-KNIGHT S.,”Myofunctional Therapy as an alternative or
support to Orthodontics”, I.A.P.N.O.R., 36-42, 1, 1996
9) FRYMANN V.M.,”Relation of disturbances of craniosacral mechanism to
symptomatology of the newborn: study of 1250 infants”, J. Am. Osteop. A. 65,1059-1075, 1966
10) GAGEY P.M., WEBER B.;” Posturologia”; Ed. Marrapese Roma,1997
11) GARLINER D., “Myofunctional Therapy”, W.B.Saunders Co., 1981
12) GARLINER D.: “Myofunctional Therapy in dental practice”;III° ed. Inst. For Myofunctional Therapy, Florida,1974
13) GARLINER D.:”Effects of unrecognized abnormal swallowing”; J. Can. Dent. Ass.,34,301-304, 1968
14) GATTI COLANGELO G., BARTOCCI FESTA F., POMANTE D., COLANGELO S.,”Valutazione clinico-radiografica dei rapporti tra dorso curvo e malocclusione”, Mondo Ortodontico, IV, 1990
15) GELB H., “Clinical management of Head, Neck, and TMJ Pain and Dysfunction”, IEA Inc. Publ.,1991
16) GRABER T.M.; “The “Three m’s”: Muscles, Malformation and Malocclusion”, Am. Jour. Orthod. 49, 418-450, 1963
17) GUAGLIO G., CATANI F.: “Influenza della deglutizione atipica sulla Cifo-scoliosi”, ICAK-E Meeting,Pisa, 4/1993
18) GUAGLIO G.:”La lingua e le sue disfunzioni in rapporto alla postura di profilo:
rapporto tra alterata postura e funzione linguale e distribuzione dei carichi
sui piedi”,Attualità dentale, n° 4-1998
19) HALATA Z., BAUMANN K.I.: “Sensory nerve endings in the hard palate and papilla incisiva of the rhesus monkey”; Anatomy and Embriology, vol.199, iss.5, pp 427-437,1999
20) HARVOLD E.P.:” The role of function in the etiology and treatment of malocclusion” Am. Jour. Orthod., 54, 883-897, 1968
21) JANSKEY Z., ZELNY A., “Investigation of the muscular forces exerted by the human tongue”, Dent. Abstr., 6:267, 1961
22) LAY E.M.;”The osteopathic management of temporo-mandibular joint disfunction. Clinical management of head, neck and TMJ pain disfunction: a multidisciplinary approach to diagnosis and treatment”, edited by Harold Gelb,D.D.S.,Philadelphia, W.B.Sauden Co. ,1985
23) LEAR C.S.C., MOORREES C..F.A.,”Bucco-lingual muscle force and dental arch form”, Am. J. Orthod. 1969
24) LEVRINI A.:”Deglutizione atipica e mioterapia funzionale”; Mondo Ortod., 3, 24- 48,1977
25) LOGEMANN J. A.,”Swallowing physiology and patho-physiology”,Otol. Clin.
N.Am.,21,4,1988
26) Mc.NAMARA J. A.:”Neuromuscolar and Skeletal adaptations to altered function in the oro-facial region”; Am. Jour. Orthod., 64, 578-606, 1973
27) PROFITT W. R.,”Muscle pressure and tooth position: A review of current research”, Aust. Orthod.,3:104, 1973
28) ROBIN P., “ La glossoptose”,G.Doin Ed. Paris, 1928
29) SMITH S.,”Muscular strenght correlated to jaw posture and the temporo-mandibular joint”, N. Y. State Dent. J., 44,278-285, 1978
30) STRAUB W. J., “The etiology of the perverted swallowing habit”,Am.J.
Orthod.,603-612, 1951
31) STRAUB W.J., “Malfunction of the tongue. Part I. The abnormal swallowing habit: Its cause, effects and results in relation to orthodontic treatment and speech therapy”, J. Am. Orthod., 46:6, 1960
32) SUBTELNY J. D.,”Malocclusion, orthodontic corrections and orofacial muscle
adaptation”, Angle Orthod.,40:170, 1970
33)SUTHERLAND W.,G.:”La sfera craniale”, Futura Publ. Soc.1998
34)UPLEDGER J.E., VREDEVOOGD J.D.; “Terapia cranio-sacrale”; Red ed.1996
35) ZANARDI M.; “Posturologia clinica osteopatica”, Ed. Marrapese, Roma,1998